Abstract
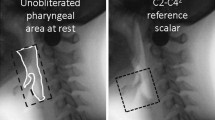
Postswallow residue is widely considered to be a sign of swallowing impairment and is assumed to pose risk for aspiration on subsequent swallows. We undertook a preliminary retrospective study to investigate the link between postswallow residue and penetration–aspiration on the immediately occurring subsequent clearing swallow (i.e., without introduction of a new bolus). Videofluoroscopy clips for 156 thin-liquid single bolus swallows by patients with neurogenic dysphagia were selected for study because they displayed multiple swallows per bolus. Residue for each subswallow (n = 407) was analyzed using the Normalized Residue Ratio Scale for the valleculae (NRRSv) and piriform sinuses. The association between residue presence at the end of a swallow and penetration–aspiration on the next swallow was examined. Postswallow residue in one or both pharyngeal spaces was significantly associated with impaired swallowing safety on the subsequent clearing swallow for the same bolus. However, when analyzed separately by residue location, only vallecular residue was significantly associated with impaired swallowing safety on the next clearing swallow. The distribution of NRRSv scores by swallowing safety demonstrated an NRRSv cut-point of 0.09, above which there was a 2.07 times greater relative risk of penetration–aspiration. Postswallow vallecular residue, measured using the NRRS, is significantly associated with penetration–aspiration on subsequent clearing swallows. A clinically meaningful cut-point of 0.09 on the NRRSv scale demarcates this risk. Further research with different bolus consistencies is needed.




Similar content being viewed by others
References
Rosenbek JC, Roecker EB, Wood JL, Robbins J. Thermal application reduces the duration of stage transition in dysphagia after stroke. Dysphagia. 1996;11:225–33.
Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin, TX: Pro-Ed; 1998.
Dodds WJ, Logemann JA, Stewart ET. Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154:965–74.
Horner J, Buoyer FG, Alberts MJ, Helms MJ. Dysphagia following brain-stem stroke. Clinical correlates and outcome. Arch Neurol. 1991;48:1170–3.
Perlman AL, Grayhack JP, Booth BM. The relationship of vallecular residue to oral involvement, reduced hyoid elevation, and epiglottic function. J Speech Hear Res. 1992;35:734–41.
Han TR, Paik N, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001;82:677–82.
Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler A, Scharitzer M, et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol. 2002;178:393–8.
Pearson WG Jr, Molfenter SM, Smith Z, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013. doi:10.1007/s00455-012-9426-9.
Ertekin C, Aydoğdu İ, Yüceyar N. Piecemeal deglutition and dysphagia limit in normal subjects and in patients with swallowing disorders. J Neurol Neurosurg Psychiatry. 1996;61:491–6.
Fink TA, Ross JB. Are we testing a true thin liquid? Dysphagia. 2009;24:285–9.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11:93–8.
Fleiss JL. The design and analysis of clinical experiments. New York: Wiley; 1986.
Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002;17:262–72.
Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Dysphagia. 2010;25:347–8.
Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006;21:270–4.
Omari TI, Dejaeger E, Van Beckevoort D, Goeleven A, De Cock P, Hoffman I, et al. A novel method for the nonradiological assessment of ineffective swallowing. Am J Gastroenterol. 2011;106:1796–802.
Ekberg O, Feinberg MJ. Altered swallowing function in elderly patients without dysphagia: Radiologic findings in 56 cases. AJR Am J Roentgenol. 1991;156:1181–4.
Acknowledgments
SMM has received funding for her doctoral studies from the Natural Sciences and Engineering Research Council (Canada) Create CARE program, the Ontario Student Opportunity Trust Fund, and the Ontario Graduate Studies scholarship program. CMS holds a New Investigator award from the Canadian Institutes of Health Research. The authors thank Becky Cliffe Polacco, Sarah Hori, Chelsea Leigh, and Clemence Tsang for assistance with data collection and analysis, and they acknowledge the support of Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-term Care in Ontario. The views expressed do not necessarily reflect those of the ministry. This work was presented in part at the 2nd European Society for Swallowing Disorders Congress on October 26, 2012 in Barcelona, Spain.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Molfenter, S.M., Steele, C.M. The Relationship Between Residue and Aspiration on the Subsequent Swallow: An Application of the Normalized Residue Ratio Scale. Dysphagia 28, 494–500 (2013). https://doi.org/10.1007/s00455-013-9459-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-013-9459-8