Abstract
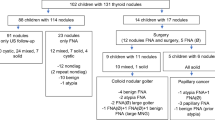
Thyroid nodules are less common in children than in adults. However, pediatric thyroid nodules have a higher rate of malignancy compared to those in adults, and increased risk of metastasis and recurrence. In the present study, we analyzed the clinical features as well as laboratory and thyroid ultrasound (US) findings of children and adolescents with thyroid nodules to identify predictive factors of thyroid cancer. We retrospectively analyzed 275 patients with thyroid nodules under 18 years of age who visited Severance Children’s Hospital between January 2005 and May 2017. Among them, 141 patients who underwent ultrasonography-guided fine needle aspiration biopsy (FNAB), and four patients without FNAB who underwent surgical resection, were included in this study. The remaining 125 patients without FNAB and five patients with follow-up loss after FNAB were excluded. Clinical, laboratory, and US data were evaluated in 145 patients to establish the potential predictive factors of thyroid cancer. Thyroid malignancies were observed in 101 patients. Grade 2 goiters were seen more often in benign nodule group. Hypoechoic nodules, nodules with microcalcifications, abnormal lymph nodes, and irregular margins were findings significantly associated with thyroid cancer. The findings of hypoechoic nodule, nodule with microcalcifications, and abnormal lymph nodes showed statistical significance in predicting thyroid cancer.
Conclusion: Hypoechoic nodules, nodules with microcalcifications, and abnormal lymph nodes are predictive factors for thyroid cancer in children. Therefore, further diagnostic evaluations, including FNAB, should be considered in patients with such findings.
What is Known: • Thyroid nodules are less common in children than in adults, but pediatric thyroid nodules have a higher rate of malignancy, and also have increased risk of metastasis and recurrence. • Research on ways to predict thyroid cancer have mostly been accomplished in adult patients, and the application of risk stratification system has not been fully satisfactory in children, which requires further studies in pediatric thyroid nodules. | |
What is New: • Hypoechoic nodules, nodules with microcalcifications, and abnormal lymph nodes are predictive factors for thyroid cancer in Korean children. |

Similar content being viewed by others
Abbreviations
- BMI :
-
Body mass index
- FNAB :
-
Fine needle aspiration biopsy
- MEN :
-
Multiple endocrine neoplasia
- PCR :
-
Polymerase chain reaction
- SDS :
-
Standard deviation score
- Tg :
-
Thyroglobulin
- TPO :
-
Thyroid peroxidase
- TSH :
-
Thyroid stimulating hormone
- US :
-
Ultrasonography
References
Kaloumenou I, Alevizaki M, Ladopoulos C, Antoniou A, Duntas LH, Mastorakos G, Chiotis D, Mengreli C, Livadas S, Xekouki P, Dacou-Voutetakis C (2007) Thyroid volume and echostructure in schoolchildren living in an iodine-replete area: relation to age, pubertal stage, and body mass index. Thyroid 17(9):875–881. https://doi.org/10.1089/thy.2006.0327
Rallison ML, Dobyns BM, Meikle AW, Bishop M, Lyon JL, Stevens W (1991) Natural history of thyroid abnormalities: prevalence, incidence, and regression of thyroid diseases in adolescents and young adults. Am J Med 91(4):363–370
Hogan AR, Zhuge Y, Perez EA, Koniaris LG, Lew JI, Sola JE (2009) Pediatric thyroid carcinoma: incidence and outcomes in 1753 patients. J Surg Res 156(1):167–172. https://doi.org/10.1016/j.jss.2009.03.098
Vergamini LB, Frazier AL, Abrantes FL, Ribeiro KB, Rodriguez-Galindo C (2014) Increase in the incidence of differentiated thyroid carcinoma in children, adolescents, and young adults: a population-based study. J Pediatr 164(6):1481–1485. https://doi.org/10.1016/j.jpeds.2014.01.059
Burman KD, Wartofsky L (2015) CLINICAL PRACTICE. Thyroid nodules. N Engl J Med 373(24):2347–2356. https://doi.org/10.1056/NEJMcp1415786
Gupta A, Ly S, Castroneves LA, Frates MC, Benson CB, Feldman HA, Wassner AJ, Smith JR, Marqusee E, Alexander EK, Barletta J, Doubilet PM, Peters HE, Webb S, Modi BP, Paltiel HJ, Kozakewich H, Cibas ES, Moore FD Jr, Shamberger RC, Larsen PR, Huang SA (2013) A standardized assessment of thyroid nodules in children confirms higher cancer prevalence than in adults. J Clin Endocrinol Metab 98(8):3238–3245. https://doi.org/10.1210/jc.2013-1796
Niedziela M (2006) Pathogenesis, diagnosis and management of thyroid nodules in children. Endocr Relat Cancer 13(2):427–453. https://doi.org/10.1677/erc.1.00882
Feinmesser R, Lubin E, Segal K, Noyek A (1997) Carcinoma of the thyroid in children--a review. J Pediatr Endocrinol Metab 10(6):561–568
Josefson J, Zimmerman D (2008) Thyroid nodules and cancers in children. Pediatr Endocrinol Rev 6(1):14–23
O'Gorman CS, Hamilton J, Rachmiel M, Gupta A, Ngan BY, Daneman D (2010) Thyroid cancer in childhood: a retrospective review of childhood course. Thyroid 20(4):375–380. https://doi.org/10.1089/thy.2009.0386
Francis GL, Waguespack SG, Bauer AJ, Angelos P, Benvenga S, Cerutti JM, Dinauer CA, Hamilton J, Hay ID, Luster M, Parisi MT, Rachmiel M, Thompson GB, Yamashita S, American Thyroid Association Guidelines Task Force (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 25(7):716–759. https://doi.org/10.1089/thy.2014.0460
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133. https://doi.org/10.1089/thy.2015.0020
Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, Panunzi C, Rinaldi R, Toscano V, Pacella CM (2002) Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab 87(5):1941–1946. https://doi.org/10.1210/jcem.87.5.8504
Mussa A, De Andrea M, Motta M, Mormile A, Palestini N, Corrias A (2015) Predictors of malignancy in children with thyroid nodules. J Pediatr 167(4):886–892.e881. https://doi.org/10.1016/j.jpeds.2015.06.026
Goldfarb M, Gondek SS, Sanchez Y, Lew JI (2012) Clinic-based ultrasound can predict malignancy in pediatric thyroid nodules. Thyroid 22(8):827–831. https://doi.org/10.1089/thy.2011.0494
Al Nofal A, Gionfriddo MR, Javed A, Haydour Q, Brito JP, Prokop LJ, Pittock ST, Murad MH (2016) Accuracy of thyroid nodule sonography for the detection of thyroid cancer in children: systematic review and meta-analysis. Clin Endocrinol 84(3):423–430. https://doi.org/10.1111/cen.12786
Cavallo A, Johnson DN, White MG, Siddiqui S, Antic T, Mathew M, Grogan RH, Angelos P, Kaplan EL, Cipriani NA (2017) Thyroid nodule size at ultrasound as a predictor of malignancy and final pathologic size. Thyroid 27(5):641–650. https://doi.org/10.1089/thy.2016.0336
Kamran SC, Marqusee E, Kim MI, Frates MC, Ritner J, Peters H, Benson CB, Doubilet PM, Cibas ES, Barletta J, Cho N, Gawande A, Ruan D, Moore FD Jr, Pou K, Larsen PR, Alexander EK (2013) Thyroid nodule size and prediction of cancer. J Clin Endocrinol Metab 98(2):564–570. https://doi.org/10.1210/jc.2012-2968
McHenry CR, Huh ES, Machekano RN (2008) Is nodule size an independent predictor of thyroid malignancy? Surgery 144(6):1062–1068; discussion 1068-1069. https://doi.org/10.1016/j.surg.2008.07.021
Papendieck P, Gruneiro-Papendieck L, Venara M, Acha O, Cozzani H, Mateos F, Maglio S, Calcagno ML, Bergada I, Chiesa A (2015) Differentiated thyroid cancer in children: prevalence and predictors in a large cohort with thyroid nodules followed prospectively. J Pediatr 167(1):199–201. https://doi.org/10.1016/j.jpeds.2015.04.041
Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, Kim J, Kim HS, Byun JS, Lee DH (2008) Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology 247(3):762–770. https://doi.org/10.1148/radiol.2473070944
Kwak JY, Han KH, Yoon JH, Moon HJ, Son EJ, Park SH, Jung HK, Choi JS, Kim BM, Kim EK (2011) Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology 260(3):892–899. https://doi.org/10.1148/radiol.11110206
Lim-Dunham JE, Toslak IE, Reiter MP, Martin B (2019) Assessment of the American college of radiology thyroid imaging reporting and data system for thyroid nodule malignancy risk stratification in a pediatric population. AJR Am J Roentgenol 212(1):188–194. https://doi.org/10.2214/ajr.18.20099
Creo A, Alahdab F, Al Nofal A, Thomas K, Kolbe A, Pittock ST (2018) Ultrasonography and the American Thyroid Association ultrasound-based risk stratification Tool: Utility in Pediatric and Adolescent Thyroid Nodules. Horm Res Paediatr 90(2):93–101. https://doi.org/10.1159/000490468
Martinez-Rios C, Daneman A, Bajno L, van der Kaay DCM, Moineddin R, Wasserman JD (2018) Utility of adult-based ultrasound malignancy risk stratifications in pediatric thyroid nodules. Pediatr Radiol 48(1):74–84. https://doi.org/10.1007/s00247-017-3974-y
Cibas ES, Ali SZ (2009) The Bethesda system for reporting thyroid cytopathology. Thyroid 19(11):1159–1165. https://doi.org/10.1089/thy.2009.0274
Committee for the Development of Growth Standard for Korean Children and Adolescents; Korean Pediatric Society, Committee for School Health and Public Health Statistics (2007) 2007 Korean children and adolescents growth standard. Korea Centers for Disease Control and Prevention, Division of Chronic Disease Surveillance, Cheongwon
Organization WH, Disorders ICfCoID, UNICEF (1994) Indicators for assessing iodine deficiency disorders and their control through salt iodization
Trahan J, Reddy A, Chang E, Gomez R, Prasad P, Jeyakumar A (2016) Pediatric thyroid nodules: A single center experience. Int J Pediatr Otorhinolaryngol 87:94–97. https://doi.org/10.1016/j.ijporl.2016.06.011
Wu XC, Chen VW, Steele B, Roffers S, Klotz JB, Correa CN, Carozza SE (2003) Cancer incidence in adolescents and young adults in the United States, 1992-1997. J Adolesc Health 32(6):405–415
Derwahl M, Nicula D (2014) Estrogen and its role in thyroid cancer. Endocr Relat Cancer 21(5):T273–T283. https://doi.org/10.1530/erc-14-0053
Imai Y, Yamakawa M, Matsuda M, Kasajima T (1989) Endogenous sex hormone and estrogen binding activity in thyroid cancer. Histol Histopathol 4(1):39–45
Vannucchi G, De Leo S, Perrino M, Rossi S, Tosi D, Cirello V, Colombo C, Bulfamante G, Vicentini L, Fugazzola L (2015) Impact of estrogen and progesterone receptor expression on the clinical and molecular features of papillary thyroid cancer. Eur J Endocrinol 173(1):29–36. https://doi.org/10.1530/eje-15-0054
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578. https://doi.org/10.1016/s0140-6736(08)60269-x
Wu C, Wang L, Chen W, Zou S, Yang A (2017) Associations between body mass index and lymph node metastases of patients with papillary thyroid cancer: A retrospective study. Medicine (Baltimore) 96(9):e6202. https://doi.org/10.1097/md.0000000000006202
Buryk MA, Simons JP, Picarsic J, Monaco SE, Ozolek JA, Joyce J, Gurtunca N, Nikiforov YE, Feldman Witchel S (2015) Can malignant thyroid nodules be distinguished from benign thyroid nodules in children and adolescents by clinical characteristics? A review of 89 pediatric patients with thyroid nodules. Thyroid 25(4):392–400. https://doi.org/10.1089/thy.2014.0312
Mussa A, Salerno MC, Bona G, Wasniewska M, Segni M, Cassio A, Vigone MC, Gastaldi R, Iughetti L, Santanera A, Capalbo D, Matarazzo P, de Luca F, Weber G, Corrias A (2013) Serum thyrotropin concentration in children with isolated thyroid nodules. J Pediatr 163(5):1465–1470. https://doi.org/10.1016/j.jpeds.2013.07.003
Chiu HK, Sanda S, Fechner PY, Pihoker C (2012) Correlation of TSH with the risk of paediatric thyroid carcinoma. Clin Endocrinol 77(2):316–322. https://doi.org/10.1111/j.1365-2265.2012.04383.x
Azizi G, Malchoff CD (2011) Autoimmune thyroid disease: a risk factor for thyroid cancer. Endocr Pract 17(2):201–209. https://doi.org/10.4158/ep10123.or
Wong SL, Grodski S, Yeung MJ, Serpell JW (2015) Anti-thyroid antibodies as a predictor of thyroid cancer. ANZ J Surg 85(11):849–853. https://doi.org/10.1111/ans.12453
Kambalapalli M, Gupta A, Prasad UR, Francis GL (2015) Ultrasound characteristics of the thyroid in children and adolescents with goiter: a single center experience. Thyroid 25(2):176–182. https://doi.org/10.1089/thy.2014.0161
Raparia K, Min SK, Mody DR, Anton R, Amrikachi M (2009) Clinical outcomes for "suspicious" category in thyroid fine-needle aspiration biopsy: Patient's sex and nodule size are possible predictors of malignancy. Arch Pathol Lab Med 133(5):787–790. https://doi.org/10.1043/1543-2165-133.5.787
Richman DM, Benson CB, Doubilet PM, Peters HE, Huang SA, Asch E, Wassner AJ, Smith JR, Cherella CE, Frates MC (2018) Thyroid nodules in pediatric patients: sonographic characteristics and likelihood of cancer. Radiology 288(2):591–599. https://doi.org/10.1148/radiol.2018171170
Sclabas GM, Staerkel GA, Shapiro SE, Fornage BD, Sherman SI, Vassillopoulou-Sellin R, Lee JE, Evans DB (2003) Fine-needle aspiration of the thyroid and correlation with histopathology in a contemporary series of 240 patients. Am J Surg 186(6):702–709 discussion 709-710
Gannon AW, Langer JE, Bellah R, Ratcliffe S, Pizza J, Mostoufi-Moab S, Cappola AR, Bauer AJ (2018) Diagnostic accuracy of ultrasound with color flow Doppler in children with thyroid nodules. J Clin Endocrinol Metab 103(5):1958–1965. https://doi.org/10.1210/jc.2017-02464
Frates MC, Benson CB, Doubilet PM, Kunreuther E, Contreras M, Cibas ES, Orcutt J, Moore FD Jr, Larsen PR, Marqusee E, Alexander EK (2006) Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 91(9):3411–3417. https://doi.org/10.1210/jc.2006-0690
Mendelson AA, Tamilia M, Rivera J, Hier MP, Sherman M, Garfield N, Black MJ, Rochon L, Gologan O, Payne RJ (2009) Predictors of malignancy in preoperative nondiagnostic biopsies of the thyroid. J Otolaryngol Head Neck Surg 38(3):395–400
Shrestha M, Crothers BA, Burch HB (2012) The impact of thyroid nodule size on the risk of malignancy and accuracy of fine-needle aspiration: a 10-year study from a single institution. Thyroid 22(12):1251–1256. https://doi.org/10.1089/thy.2012.0265
Lyshchik A, Drozd V, Demidchik Y, Reiners C (2005) Diagnosis of thyroid cancer in children: value of gray-scale and power doppler US. Radiology 235(2):604–613. https://doi.org/10.1148/radiol.2352031942
Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, Cronan JJ, Doubilet PM, Evans DB, Goellner JR, Hay ID, Hertzberg BS, Intenzo CM, Jeffrey RB, Langer JE, Larsen PR, Mandel SJ, Middleton WD, Reading CC, Sherman SI, Tessler FN (2006) Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Ultrasound Q 22(4):231–238; discussion 239-240. https://doi.org/10.1097/01.ruq.0000226877.19937.a1
Frates MC, Benson CB, Doubilet PM, Cibas ES, Marqusee E (2003) Can color Doppler sonography aid in the prediction of malignancy of thyroid nodules? J Ultrasound Med 22(2):127–131 quiz 132-124
Demidchik YE, Demidchik EP, Reiners C, Biko J, Mine M, Saenko VA, Yamashita S (2006) Comprehensive clinical assessment of 740 cases of surgically treated thyroid cancer in children of Belarus. Ann Surg 243(4):525–532. https://doi.org/10.1097/01.sla.0000205977.74806.0b
Park S, Jeong JS, Ryu HR, Lee CR, Park JH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2013) Differentiated thyroid carcinoma of children and adolescents: 27-year experience in the Yonsei University Health System. J Korean Med Sci 28(5):693–699. https://doi.org/10.3346/jkms.2013.28.5.693
Elisei R, Ugolini C, Viola D, Lupi C, Biagini A, Giannini R, Romei C, Miccoli P, Pinchera A, Basolo F (2008) BRAF(V600E) mutation and outcome of patients with papillary thyroid carcinoma: a 15-year median follow-up study. J Clin Endocrinol Metab 93(10):3943–3949. https://doi.org/10.1210/jc.2008-0607
Xing M (2005) BRAF mutation in thyroid cancer. Endocr Relat Cancer 12(2):245–262. https://doi.org/10.1677/erc.1.0978
Henke LE, Perkins SM, Pfeifer JD, Ma C, Chen Y, DeWees T, Grigsby PW (2014) BRAF V600E mutational status in pediatric thyroid cancer. Pediatr Blood Cancer 61(7):1168–1172. https://doi.org/10.1002/pbc.24935
Chow SM, Law SC, Mendenhall WM, Au SK, Yau S, Mang O, Lau WH (2004) Differentiated thyroid carcinoma in childhood and adolescence-clinical course and role of radioiodine. Pediatr Blood Cancer 42(2):176–183. https://doi.org/10.1002/pbc.10410
Welch Dinauer CA, Tuttle RM, Robie DK, McClellan DR, Svec RL, Adair C, Francis GL (1998) Clinical features associated with metastasis and recurrence of differentiated thyroid cancer in children, adolescents and young adults. Clin Endocrinol 49(5):619–628
Zimmerman D, Hay ID, Gough IR, Goellner JR, Ryan JJ, Grant CS, McConahey WM (1988) Papillary thyroid carcinoma in children and adults: long-term follow-up of 1039 patients conservatively treated at one institution during three decades. Surgery 104(6):1157–1166
Handkiewicz-Junak D, Wloch J, Roskosz J, Krajewska J, Kropinska A, Pomorski L, Kukulska A, Prokurat A, Wygoda Z, Jarzab B (2007) Total thyroidectomy and adjuvant radioiodine treatment independently decrease locoregional recurrence risk in childhood and adolescent differentiated thyroid cancer. J Nucl Med 48(6):879–888. https://doi.org/10.2967/jnumed.106.035535
Author information
Authors and Affiliations
Contributions
Junghwan Suh, Ahreum Kwon, and Ho-Seong Kim designed the study, Junghwan Suh, Han Saem Choi, and Hyun Wook Chae analyzed the data, and the script is written by Junghwan Suh.
Corresponding author
Ethics declarations
This study was approved by the institutional review board of Severance Hospital, Yonsei University College of Medicine in Seoul, Korea (no. 4-2017-1216).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The requirement to obtain informed consent was waived.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suh, J., Choi, H.S., Kwon, A. et al. Adolescents with thyroid nodules: retrospective analysis of factors predicting malignancy. Eur J Pediatr 179, 317–325 (2020). https://doi.org/10.1007/s00431-019-03507-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03507-4