Abstract
In patients with a single functioning kidney, renal function was assessed at regular intervals over a period of 10 years. Serum creatinine, glomerular filtration rate (GFR), blood pressure, and urinary protein–creatinine ratio were assessed at the age of 2, 5 and 10 years. Between January 1980 and December 2005, 99 such patients were diagnosed in the first year of life. They were divided into three groups: A, patients with multicystic kidney disease and a normal contralateral kidney (n = 36); B, patients with a normal solitary kidney without uropathy (n = 20); and C, patients with obstructive uropathy and one nonfunctioning kidney (n = 43). Serum creatinine levels increased significantly with increasing age in every group. In group C, serum creatinine was significantly elevated compared with group A in all age categories (p = 0.043, p = 0.019, p = 0.001 respectively). Median figures of GFR remained within normal limits over the 10-year period. GFR was significantly lower in group C compared with group A (p = 0.001, p = 0.009, p = 0.019 respectively) and B in all age categories (p = 0.013, p = 0.002, p = 0.016 respectively). There were no changes in blood pressure over time and no differences among the three groups were observed. At the age of 10 years, the patients in group C had a significantly higher median urinary protein–creatinine ratio (p = 0.022) than those in groups A and B. There was also an increasing level of proteinuria with increasing age in group C (p = 0.002). In conclusion, renal function was stable over time in all patients, but children with obstructive uropathy have a lower median GFR and higher serum creatinine level for the whole study period. Hypertension was exceptionally observed in group C, with obstructive uropathy, as was an elevated urinary protein–creatinine ratio.
Similar content being viewed by others
Introduction
A reduction in renal mass leads to adaptation in the remaining nephrons. Beyond a certain limit, adaptation results in progression due to glomerular hyperperfusion, hyperfiltration, and hypertension, leading to a gradual decline in renal function [6]. Progression is characterized by proteinuria, hypertension, and a gradual drop in the glomerular filtration rate. This phenomenon is well documented in experimental models and a number of human disorders with reduced renal mass. In this study we asked the following question: does progression occur in patients with a single functioning kidney from birth within a period of 10 years?
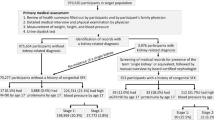
Patients and methods
In the Renal Unit of our Department of Pediatrics, all patients with a single functioning kidney underwent renal function evaluation at the age of 2, 5 and 10 years. Physical examination included three blood pressure measurements, the average of which was expressed as age-related percentiles according to the American Task Force on Blood Pressure Control in Children [1]. In a urine sample the protein–creatinine ratio was measured and expressed as milligram per milligram (mg/mg), the normal value being <0.5 in infants and <0.25 beyond infancy. Serum creatinine was measured and expressed in milligram per deciliter (mg/dl). The glomerular filtration rate was measured as inulin clearance using the single shot technique and, once the children were continent, as creatinine clearance measured in 24-h urine collections.
In this paper we summarize our findings in 99 patients with a single functioning kidney observed in our renal unit over the past 25 years. All patients were diagnosed in the first year of life. Ultrasonography was used to define “normal” kidneys and multicystic kidney disease. Isotope scintigraphy was used to identify nonfunctioning kidneys (technetium-99m dimercaptosuccinic acid) and obstructed urinary tracts (technetium-99m mercaptoacetyltriglycine). Traditional voiding cystography was used to document vesico-ureteral reflux and the urethral valves. Patients were divided into three subgroups: A, patients with multicystic kidney disease (MCKD) having a normal contralateral kidney; B, patients with a normal solitary kidney without uropathy; C, patients with a nonfunctioning kidney within the framework of obstructive uropathy: grade IV and V vesico-ureteral reflux (VUR), ureteropelvic junction obstruction (UPJO), ureterovesical obstruction (UVJO), and posterior urethral valves. Patients with an underlying syndrome or other malformations were excluded, e.g. VATER sequence, Turner syndrome, tuberous sclerosis, etc. The Kruskal–Wallis analysis of variance or Mann–Whitney U test were used to analyze the differences among groups A, B, and C. The changes that occurred over 10 years in the patients were analyzed using the paired signed rank test. A p value <0.05 was considered statistically significant.
Results
Patients’ characteristics
Table 1 shows the number of patients according to subgroups and ages at investigation.
Group A included 36 patients (23 boys). The multicystic dysplastic kidney was on the left side in 18 patients. Nephrectomy was performed in 4 patients. The following extrarenal abnormalities were present: ventricular septum defect (n = 1), undescended testicle (n = 3), hypospadias (n = 1), and inguinal hernia (n = 3). Urinary tract infections were documented in 3 patients.
Group B consisted of 20 patients (15 boys). The solitary kidney was left-sided in 11 patients. In 5 children there was an extrarenal anomaly: coarctation of the aorta (n = 1), undescended testicle (n = 3), and ureterocele (n = 1). In 1 patient a urinary tract infection was documented.
Group C was made up of 43 patients (27 boys). The nonfunctional kidney was on the left side in 22 patients. It had been removed in 11 children. VUR was observed in 27 patients; it was bilateral in 9 and surgically corrected in 13 children. UPJO was present in 7 patients, UVJO in 4, and urethral valves in another 5 patients. The latter patients had undergone surgery at least once. Extrarenal anomalies were undescended testicle (n = 3) and inguinal hernia (n = 1). Urinary tract infection was documented in 9 patients.
The records of the 10-year-old patients are incomplete because they did not appear at follow-up or were not yet 10 years old (see Table 1) at the time of writing.
Serum creatinine
The increase in serum creatinine levels with increasing age was statistically significant in every group. Group C had a significantly higher median creatinine level in all age categories compared with group A (p < 0.005, p < 0.05, p < 0.005 respectively). At the age of 10 years, the creatinine level was significantly lower in group A compared with patients in group B (p < 0.05); Fig. 1.
Glomerular filtration rate (ml/min per 1.73 m2)
Median glomerular filtration rate (GFR) did not change over time. Group C had a significantly lower GFR compared with group A (p < 0.005, p < 0.05, p < 0.05) respectively and B (p < 0.05, p < 0.005, p < 0.05) at every age (Fig. 1).
In group A, GFR was below 80 ml/min per 1.73 m2 in 2 out of 36 patients at 2 years, in 4 out of 36 patients at 5 years and in 2 out of 16 patients at 10 years. In group B, we noticed a GFR below 80 ml/min per 1.73 m2 in 3 out of 20 patients at 2 years, in 2 out of 20 patients at 5 years and in 1 out of 16 patients at 10 years. In group C, GFR was below 80 ml/min per 1.73 m2 in 14 out of 43 patients at 2 years, in 16 out of 43 patients at 5 years and in 9 out of 31 patients at 10 years.
Blood pressure
In the vast majority of patients studied over the 10-year period, systolic and diastolic blood pressure was below the 95th percentile. Median blood pressure figures did not increase with age. There were no significant differences among the three groups (Table 2).
Urinary protein–creatinine ratio
A urinary protein–creatinine ratio >0.25 mg/mg was surprisingly more frequent at the age of 2 years in all three subgroups of patients than later in life, whereas a ratio >0.5 mg/mg was only seen in group C. At 5 and 10 years of age, proteinuria was exceptional in groups A and B, but present in 12 out of 31 patients in group C. In group C, proteinuria increased significantly with age (p < 0.005); Table 3).
Discussion
In this study we assessed serum creatinine levels, GFR measured with inulin or creatinine, blood pressure, and urinary protein excretion in 99 pediatric patients with a single functioning kidney which was a normal as judged by ultrasound. These patients, who were diagnosed in the first year of life, were studied at the age 2, 5, and 10 years. The cohort was subdivided into three subgroups according to the underlying disorder: multicystic kidneys (A), solitary kidneys (B), and obstructive uropathy (C). Low GFR, hypertension, and proteinuria were abnormalities found in all three subgroups, but with a significantly higher rate in subgroup C. This is no surprise since patients with obstructive uropathy are likely to be at risk of a contralateral anomaly. Yet, it is important to note that patients in groups A and B were not necessarily without anomalies. These patients were born with one functioning kidney. The main question is: are they at risk of progression? In other words, do they have a reduced number of nephrons?
Having one kidney from birth does not necessarily mean a reduced number of nephrons. It is likely that single kidneys can have extra nephrons as a consequence of intrauterine adaptation of nephrogenesis. This is suggested by findings in human beings [8, 12] and has been documented by elegant experiments in the lamb [7]. Nevertheless, the high incidence of a contralateral anomaly in patients with MCKD explains the variability of renal anomalies at follow-up [10].
There are a large number of publications on the long-term sequelae of nephrectomy in healthy kidney donors and for the sake of conciseness only two are mentioned here [9, 17]. It is felt that this very specific topic does not fall within the scope of this paper.
To our knowledge, nine more or less comparable studies on the fate of solitary kidneys occurring in childhood have been published over the past 22 years (Table 4) [2–5, 11–14, 16]. These studies, however, are difficult to compare for several reasons: the number of individuals studied varied considerably (from 27 to 202) as do the underlying kidney disorders (from MCKD over urethral valves to Wilms’ tumor) and the length of follow-up (from months to decades). Most studies are cross-sectional and there are major differences in methodology. In six reports GFR was measured either as creatinine clearance or inulin clearance, but in three GFR was estimated using the Schwartz formula (based on serum creatinine and body length), which is less accurate. Proteinuria was not included in one study, was assessed by dipstix in two studies, by urinary protein–creatinine ratio in two other studies, and measured in urine collection in the remaining studies. Lastly, the data are presented differently: sometimes as means and SD, sometimes as absolute values with or without ranges.
Yet, all studies indicate that, in a variable percentage of patients, there are problems in terms of reduced GFR, arterial hypertension, and proteinuria. The earliest study, by Robitaille et al., is instructive [14]. Patients undergoing unilateral nephrectomy at a young age were studied as young adults. A reduced GFR was found in 3 out of 27, and proteinuria was found in 3 out of 27 former patients. The study that illustrates the best the risks related to solitary kidneys is the one by Baudoin et al. [5] on a heterogeneous cohort of 111 patients who underwent unilateral nephrectomy before the age of 16 years. The authors clearly demonstrate that the incidence of reduced GFR, hypertension, and proteinuria increases over time to become striking with a follow-up of over 25 years.
Only two studies are comparable to ours, since they include only pediatric patients followed longitudinally. Aslam et al. studied 165 children with MCKD [4]. At the age of 10 years, none had hypertension or proteinuria, but the estimated GFR was between 48 and 125 ml/min per 1.73 m2 with 2 out of 31 patients below 60 ml/min per 1.73 m2. Wilson et al. studied a mixed cohort of 74 patients followed over time [18]. These authors did not evaluate proteinuria or blood pressure; GFR measured as inulin clearance was below 85 ml/min per 1.73 m2 in 16 out of 74 patients. Seeman et al. were the only authors to distinguish between normal and abnormal solitary kidneys [15]. As in our study, it was shown that abnormalities were detected mainly in the latter.
Only two studies provide blood pressure data collected by 24-h ambulatory blood pressure measurement (ABPM), which is considered to be the optimal approach to hypertension in general, and to screen for blood pressure problems [13, 15].
From our study, and from other studies, it seems reasonable that individuals with a single functioning kidney for whatever reason deserve long-term follow-up during and after childhood. Additional prospective carefully designed studies are needed to identify those at risk of a progressive decrease in GFR, of which proteinuria and hypertension are the hallmarks. Studies could be optimized in several ways and these are our recommendations.
-
1.
All patients born with a single functioning kidney deserve follow-up at regular intervals during and beyond childhood. The age of 2 years is an excellent moment to evaluate the kidney, which by that time has matured. The next step depends on what is found at age 2 years, but, as our study points out, ages 5 and 10 years are likely to be well chosen for the purpose.
-
2.
Blood pressure should be measured, the best technique being the ABPM over a 24-h period [13]. Yet, this is hard to carry out at a young age and normal values are lacking at this time.
-
3.
Urinalysis should include measuring proteinuria. The easiest way is measuring the protein–creatinine ratio in a random sample. More sensitive is microalbuminuria, which can also be estimated as a ratio over creatinine in a sample, but preferably in timed collections, as is done in children with diabetes mellitus. Microalbuminuria is a more sensitive marker for nephron hypertrophy and hyperfiltration.
-
4.
Glomerular function needs to be estimated. Measuring serum creatinine is elementary, but not enough. For continent children, creatinine clearance measured in 24-hr urine collection is good enough for clinical studies. Other clearance techniques using inulin, iothalamate or chromium EDTA are better, especially in young patients.
-
5.
Imaging is useful to distinguish between normal and abnormal kidneys. We would like to suggest ultrasound for measuring kidney volume rather than kidney length.
-
6.
If signs of progression are documented, treatment with either an angiotensin-converting enzyme inhibitor or an angiotensin receptor antagonist is indicated. It is good to remember that a renal artery stenosis on a single kidney is a contraindication for the use of these drugs.
Abbreviations
- ABPM:
-
ambulatory blood pressure measurement
- GFR:
-
glomerular filtration rate
- MCKD:
-
multicystic kidney disease
- Up/c:
-
urinary protein–creatinine ratio
- UPJO:
-
ureteropelvic junction obstruction
- UVJO:
-
ureterovesical junction obstruction
- VUR:
-
vesico-ureteral reflux
References
Anonymous (1987) Report of the second task force on blood pressure control in children. Pediatrics 79:1–25
Argueso LR, Ritchey ML, Boyle ET Jr, Milliner DS, Bergstralh EJ, Kramer SA (1992) Prognosis of children with solitary kidney after unilateral nephrectomy. J Urol 148:747–751
Argueso LR, Ritchey ML, Boyle ET Jr, Milliner DS, Bergstralh EJ, Kramer SA (1992) Prognosis of patients with unilateral agenesis. Pediatr Nephrol 6:412–416
Aslam M, Watson AR (2006) Unilateral multicystic dysplastic kidney: long term outcomes. Arch Dis Child 91:820–823
Baudoin P, Provoost AP, Molenaar JC (1993) Renal function up to 50 years after unilateral nephrectomy in childhood. Am J Kidney Dis 21:603–611
Brenner BM, Lawler EV, Mackenzie HS (1996) The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49:1774–1777
Douglas-Denton R, Moritz KM, Bertram JF, Wintour EM (2002) Compensatory renal growth after unilateral nephrectomy in the ovine fetus. J Am Soc Nephrol 13:406–410
Glazebrook K, McGrath F, Steele BT (1993) Prenatal compensatory renal growth: documentation with US. Radiology 189:733–735
Heymans C, Breysem L, Proesmans W (1998) Multicystic kidney dysplasia: a prospective study on the natural history of the affected and contralateral kidney. Eur J Pediatr 156:673–675
Higashihara E, Horie S, Takeuchi T, Nutahara K, Aso Y (1990) Long term consequence of nephrectomy. J Urol 143:239–243
Kuwertz-Broeking E, Brinkmann OA, Von Lengerke HJ, Sciuk J, Fruend S, Bulla M, Harms E, Hertle L (2004) Unilateral multicystic dysplastic kidney: experience in children. BJU Int 93:388–392
Maluf NS (1997) On the enlargement of the normal congenitally solitary kidney. Br J Urol 79:836–841
Mei-Zahav M, Korzets Z, Cohen I, Kessler O, Rathaus V, Wolach B, Pomeranz A (2001) Ambulatory blood pressure monitoring in children with a solitary kidney—a comparison between unilateral renal agenesis and uninephrectomy. Blood Press Monit 6:263–267
Robitaille P, Lortie L, Mongeau JG, Sinnassamy P (1985) Long-term follow-up of patients who underwent unilateral nephrectomy in childhood. Lancet 8:1297–1299
Seeman T, Patzer L, John U, Dusek J, Vondrak K, Janda J, Misselwitz J (2006) Blood pressure, renal function, and proteinuria in children with unilateral renal agenesis. Kidney Blood Press Res 29:210–215
Wikstad I, Celsi G, Larssoon L, Herin P, Aperia A (1988) Kidney function in adults born with unilateral renal agenesis or nephrectomized in childhood. Pediatr Nephrol 2:177–182
Williams SL, Oler J, Jorkasky DK (1986) Long-term renal function in kidney donors: a comparison of donors and their siblings. Ann Intern Med 105:1–8
Wilson BE, Davie P, Shah K, Wong W, Taylor CM (2003) Renal length and inulin clearance in the radiologically normal single kidney. Pediatr Nephrol 18:1147–1151
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vu, KH., Van Dyck, M., Daniels, H. et al. Renal outcome of children with one functioning kidney from birth. A study of 99 patients and a review of the literature. Eur J Pediatr 167, 885–890 (2008). https://doi.org/10.1007/s00431-007-0612-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-007-0612-y