Abstract
Background
Previous studies reported that the thickness of the macular ganglion cell complex (mGCC) showed good diagnostic ability for detecting glaucoma. However, its impact on the progression of visual field loss in primary open angle glaucoma (POAG) is unknown. The purpose of this study was to assess whether baseline mGCC thickness is associated with the progression of visual field loss in POAG.
Methods
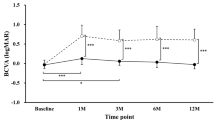
Fifty-six patients with POAG were included in the study. All patients were followed for more than 2 years after baseline optical coherence tomography (OCT) measurements. They had at least five reliable Humphrey visual field tests with 30–2 Swedish Interactive Threshold Algorithm standard tests during the follow-up period. The subjects were divided into two groups according to the slope of the mean deviation (MD): the fast progression group (MD slope < −0.4 dB/y) and the slow progression group (MD slope ≥ −0.4 dB/y). Factors compared between the groups were as follows: age, baseline intraocular pressure (IOP), mean IOP during the follow-up, refraction, baseline MD, pattern standard deviation (PSD), and baseline OCT measurements.
Results
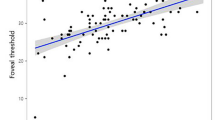
There were no significant differences between the two groups in age, baseline IOP, mean IOP during the follow-up, refraction, baseline MD or PSD, average thickness of retinal nerve fiber layer (RNFL), or disc parameters. However, the baseline mGCC thickness (average and inferior hemifield) was significantly thinner in the fast progression group than in the slow progression group (74.0 ± 7.2 μm vs. 80.3 ± 8.6 μm; 68.0 ± 6.6 μm vs. 78.2 ± 11.6 μm, respectively). Moreover, global loss volume and focal loss volume, which are parameters of mGCC, showed significantly higher rates in the fast progression group than in the slow progression group. In multivariate analysis, only mGCC thickness of the inferior hemifield was associated with disease progression (P = 0.007).
Conclusions
Baseline mGCC thickness can be predictive of progressive visual field loss in patients with POAG.


Similar content being viewed by others
References
Quigley HA, Addicks EM, Green WR (1982) Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol 100:135–146
Quigley HA, Dunkelberger GR, Green WR (1989) Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol 107:453–464
Tan O, Chopra V, Lu AT, Schuman JS, Ishikawa H, Wollstein G, Varma R, Huang D (2009) Detection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomography. Ophthalmology 116:2305–2314, e1-2
Airaksinen PJ, Drance SM, Douglas GR, Mawson DK, Nieminen H (1984) Diffuse and localized nerve fiber loss in glaucoma. Am J Ophthalmol 98:566–571
Quigley HA, Katz J, Derick RJ, Gilbert D, Sommer A (1992) An evaluation of optic disc and nerve fiber layer examinations in monitoring progression of early glaucoma damage. Ophthalmology 99:19–28
Sommer A, Katz J, Quigley HA, Miller NR, Robin AL, Richter RC, Witt KA (1991) Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol 109:77–83
Harwerth RS, Carter-Dawson L, Shen F, Smith EL 3rd, Crawford ML (1999) Ganglion cell losses underlying visual field defects from experimental glaucoma. Investig Ophthalmol Vis Sci 40:2242–2250
Kim NR, Lee ES, Seong GJ, Kim JH, An HG, Kim CY (2010) Structure-function relationship and diagnostic value of macular ganglion cell complex measurement using Fourier-domain OCT in glaucoma. Investig Ophthalmol Vis Sci 51:4646–4651
Seong M, Sung KR, Choi EH, Kang SY, Cho JW, Um TW, Kim YJ, Park SB, Hong HE, Kook MS (2010) Macular and peripapillary retinal nerve fiber layer measurements by spectral domain optical coherence tomography in normal-tension glaucoma. Investig Ophthalmol Vis Sci 51:1446–1452
Schulze A, Lamparter J, Pfeiffer N, Berisha F, Schmidtmann I, Hoffmann EM (2011) Diagnostic ability of retinal ganglion cell complex, retinal nerve fiber layer, and optic nerve head measurements by Fourier-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 249:1039–1045
Rolle T, Briamonte C, Curto D, Grignolo FM (2011) Ganglion cell complex and retinal nerve fiber layer measured by fourier-domain optical coherence tomography for early detection of structural damage in patients with preperimetric glaucoma. Clin Ophthalmol 5:961–969
Naghizadeh F, Garas A, Vargha P, Hollo G (2012) Detection of early glaucomatous progression with different parameters of the RTVue optical coherence tomograph. J Glaucoma
Sung KR, Kim S, Lee Y, Yun SC, Na JH (2011) Retinal nerve fiber layer normative classification by optical coherence tomography for prediction of future visual field loss. Investig Ophthalmol Vis Sci 52:2634–2639
Lalezary M, Medeiros FA, Weinreb RN, Bowd C, Sample PA, Tavares IM, Tafreshi A, Zangwill LM (2006) Baseline optical coherence tomography predicts the development of glaucomatous change in glaucoma suspects. Am J Ophthalmol 142:576–582
Sehi M, Bhardwaj N, Chung YS, Greenfield DS, Advanced Imaging for Glaucoma Study Group (2012) Evaluation of baseline structural factors for predicting glaucomatous visual-field progression using optical coherence tomography, scanning laser polarimetry and confocal scanning laser ophthalmoscopy. Eye (Lond) 26:1527–1535
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M, Early Manifest Glaucoma Trial Group (2002) Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 120:1268–1279
Anderson DR, Drance SM, Schulzer M, Collaborative Normal-Tension Glaucoma Study Group (2001) Natural history of normal-tension glaucoma. Ophthalmology 108:247–253
Fukuchi T, Yoshino T, Sawada H, Seki M, Togano T, Tanaka T, Ueda J, Abe H (2010) Progression rate of total, and upper and lower visual field defects in open-angle glaucoma patients. Clin Ophthalmol 4:1315–1323
Kita Y, Kita R, Nitta A, Nishimura C, Tomita G (2011) Glaucomatous eye macular ganglion cell complex thickness and its relation to temporal circumpapillary retinal nerve fiber layer thickness. Jpn J Ophthalmol 55:228–234
Lee J, Hangai M, Kimura Y, Takayama K, Kee C, Yoshimura N (2013) Measurement of macular ganglion cell layer and circumpapillary retinal nerve fiber layer to detect paracentral scotoma in early glaucoma. Graefes Arch Clin Exp Ophthalmol 251:2003–2012
Takagi ST, Kita Y, Yagi F, Tomita G (2011) Macular retinal ganglion cell complex damage in the apparently normal visual field of glaucomatous eyes with hemifield defects. J Glaucoma 21:318–325
Leung CK, Cheung CY, Weinreb RN, Qiu K, Liu S, Li H, Xu G, Fan N, Pang CP, Tse KK, Lam DS (2010) Evaluation of retinal nerve fiber layer progression in glaucoma: a study on optical coherence tomography guided progression analysis. Investig Ophthalmol Vis Sci 51:217–222
Lee EJ, Kim TW, Weinreb RN, Park KH, Kim SH, Kim DM (2011) Trend-based analysis of retinal nerve fiber layer thickness measured by optical coherence tomography in eyes with localized nerve fiber layer defects. Investig Ophthalmol Vis Sci 52:1138–1144
Leung CK, Yu M, Weinreb RN, Lai G, Xu G, Lam DS (2012) Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: patterns of retinal nerve fiber layer progression. Ophthalmology 119:1858–1866
Medeiros FA, Zangwill LM, Alencar LM, Bowd C, Sample PA, Susanna R Jr, Weinreb RN (2009) Detection of glaucoma progression with stratus OCT retinal nerve fiber layer, optic nerve head, and macular thickness measurements. Investig Ophthalmol Vis Sci 50:5741–5748
Rao HL, Zangwill LM, Weinreb RN, Sample PA, Alencar LM, Medeiros FA (2010) Comparison of different spectral domain optical coherence tomography scanning areas for glaucoma diagnosis. Ophthalmology 117:1692–1699, 1699.e1
Acknowledgments
The authors received no financial support, and declare that they have no financial conflicts of interests.
Conflict of interest
The authors have no proprietary interests in any of the material used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anraku, A., Enomoto, N., Takeyama, A. et al. Baseline thickness of macular ganglion cell complex predicts progression of visual field loss. Graefes Arch Clin Exp Ophthalmol 252, 109–115 (2014). https://doi.org/10.1007/s00417-013-2527-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2527-9