Abstract
Introduction
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease with loss of muscle function. The pathogenesis is still unclear and the heterogeneity of ALS phenotypes is huge. We investigated a large population of ALS patients and controls concerning comorbidities and medications to detect specific risk or protective factors regarding onset and progression of ALS.
Methods
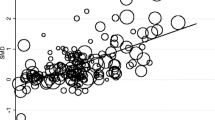
We investigated a cohort of 200 ALS patients pro- and retrospectively compared to a control group. For comparison of frequencies of comorbidities and medication intake, uni- and multivariate binary logistic regressions were performed. To analyze the influence of comorbidities and medication on the progression of ALS, we used linear regression analysis.
Results
ALS patients showed a relevantly higher prevalence of strokes and depression compared to controls. Moreover, ALS patients reported relevantly more often regular physical activity and their BMI was lower. The coexistence of coronary heart disease was associated with a relevantly faster disease progression. Intake of contraceptives was relevantly higher in controls compared with ALS patients.
Conclusions
Our results suggest stroke, lower BMI, and regular physical activity as risk factors for ALS. Strokes could be a possible trigger of the pathogenetic pathway of ALS and the lower BMI with consecutively lower rate of hyperlipidemia supports the hypothesis of premorbid hypermetabolism in ALS patients. Coexistence of coronary heart disease possibly has a negative influence on respiratory involvement. Contraceptives could be beneficial due to a protective effect of estrogen. Information on influencing factors can help to elucidate the pathogenesis of ALS or provide approaches for possible therapeutic options.


Similar content being viewed by others
References
Silani V, Ludolph A, Fornai F (2017) The emerging picture of ALS: A multisystem, not only a “motor neuron disease”. Arch Ital Biol 155:99–109
Gallo V, Wark PA, Jenab M et al (2013) Prediagnostic body fat and risk of death from amyotrophic lateral sclerosis: The EPIC cohort. Neurology 80:829–838
O’Reilly ÉJ, Wang H, Weisskopf MG et al (2013) Premorbid body mass index and risk of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 14:205–211. https://www.ncbi.nlm.nih.gov/pubmed/23134505
Dorst J, Kühnlein P, Hendrich C, Kassubek J, Sperfeld AD (2011) Ludolph AC (2011) Patients with elevated triglyceride and cholesterol serum levels have a prolonged survival in amyotrophic lateral sclerosis. J Neurol 258:613–617
Dupuis L, Corcia P, Fergani A et al (2008) Dyslipidemia is a protective factor in amyotrophic lateral sclerosis symbol. Neurology 70(13):1004–1009
Körner S, Kollewe K, Ilsemann J et al (2013) (2013) Prevalence and prognostic impact of comorbidities in amyotrophic lateral sclerosis. Eur J Neurol 20:647–654
Moglia C, Calvo A, Canosa A et al (2017) Influence of arterial hypertension, type 2 diabetes and cardiovascular risk factors on ALS outcome: a population-based study. Amyotroph Lateral Scler Front Degener 18:590–597
Turner MR, Wotton C, Talbot K, Goldacre MJ (2012) Cardiovascular fitness as a risk factor for amyotrophic lateral sclerosis: Indirect evidence from record linkage study. J Neurol Neurosurg Psychiatry 83:395–398
Harwood CA, Westgate K, Gunstone S et al (2016) Long-term physical activity: an exogenous risk factor for sporadic amyotrophic lateral sclerosis? Amyotroph Lateral Scler Front Degener 17:377–384
Longstreth WT, McGuire V, Koepsell TD, Wang Y, van Belle G (1998) Risk of amyotrophic lateral sclerosis and history of physical activity: a population-based case-control study. Arch Neurol 55:201–206. https://www.ncbi.nlm.nih.gov/pubmed/9482362
Patel BP, Hamadeh MJ (2009) Nutritional and exercise-based interventions in the treatment of amyotrophic lateral sclerosis. Clin. Nutr 28:604–617
Carreras I, Yuruker S, Aytan N et al (2010) Moderate exercise delays the motor performance decline in a transgenic model of ALS. Brain Res 1313:192–201
Prell T, Gaur N, Stubendorff B, Rödiger A, Witte OW, Grosskreutz J (2019) Disease progression impacts health-related quality of life in amyotrophic lateral sclerosis. J Neurol Sci 397:92–95. https://www.ncbi.nlm.nih.gov/pubmed/30597420
Korner S, Kammeyer J, Zapf A et al (2019) Influence of environment and lifestyle on incidence and progress of amyotrophic lateral sclerosis in A German ALS population. Aging Dis Int Soc Aging Dis 10:205–216
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169(1–2):3–21
Hollinger SK, Okosun IS, Mitchell CS (2016) Antecedent disease and amyotrophic lateral sclerosis: What is protecting whom? Front Neurol 7:47
Beghi E, Logroscino G, Chiò A et al (2010) Amyotrophic lateral sclerosis, physical exercise, trauma and sports: results of a population-based pilot case-control study. Amyotroph Lateral Scler 11:289–292
Pupillo E, Messina P, Giussani G et al (2014) Physical activity and amyotrophic lateral sclerosis: a European population-based case-control study. Ann Neurol 75:708–716. https://www.ncbi.nlm.nih.gov/pubmed/24706338.
Abel EL (2007) Football increases the risk for Lou Gehrig’s disease, amyotrophic lateral sclerosis. Percept Mot Skills 104:1251–1254
Chiò A, Benzi G, Dossena M, Mutani R, Mora G (2005) Severely increased risk of amyotrophic lateral sclerosis among Italian professional football players. Brain 128:472–476
Huisman MHB, Seelen M, De Jong SW et al (2013) Lifetime physical activity and the risk of amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 84:976–981
Mattsson P, Lönnstedt I, Nygren I, Askmark H (2012) Physical fitness, but not muscle strength, is a risk factor for death in amyotrophic lateral sclerosis at an early age. J Neurol Neurosurg Psychiatry 83:390–394
Seelen M, van Doormaal PTC, Visser AE et al (2014) Prior medical conditions and the risk of amyotrophic lateral sclerosis. J Neurol 261:1949–1956
Sutedja NA, Van Der Schouw YT, Fischer K et al (2011) Beneficial vascular risk profile is associated with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 82:638–642
Desport JC, Preux PM, Truong TC, Vallat JM, Sautereau D, Couratier P (1999) Nutritional status is a prognostic factor for survival in ALS patients. Neurology 53:1059–1063
Jawaid A, Murthy SB, Wilson AM et al (2010) A decrease in body mass index is associated with faster progression of motor symptoms and shorter survival in ALS. Amyotroph Lateral Scler 11:542–548. https://www.ncbi.nlm.nih.gov/pubmed/20500116
Dupuis L, Oudart H, René F, Gonzalez De Aguilar JL, Loeffler JP (2004) Evidence for defective energy homeostasis in amyotrophic lateral sclerosis: Benefit of a high-energy diet in a transgenic mouse model. Proc Natl Acad Sci USA 101:11159–11164
Dardiotis E, Siokas V, Sokratous M et al (2018) Body mass index and survival from amyotrophic lateral sclerosis. Neurol Clin Pract 8:437–444
Moura MC, Novaes MRCG, Eduardo EJ, Zago YSSP, Freitas RDNB, Casulari LA (2015) Prognostic factors in amyotrophic lateral sclerosis: a population-based study. PLoS One 10:e0141500. https://www.ncbi.nlm.nih.gov/pubmed/26517122
Dedic SIK, Stevic Z, Dedic V, Stojanovic VR, Milicev M, Lavrnic D (2012) Is hyperlipidemia correlated with longer survival in patients with amyotrophic lateral sclerosis? Neurol Res 34:576–580
Dupuis L, Pradat PF, Ludolph AC, Loeffler JP (2011) Energy metabolism in amyotrophic lateral sclerosis. Lancet Neurol 10:75–82
Bouteloup C, Desport J-C, Clavelou P et al (2009) Hypermetabolism in ALS patients: an early and persistent phenomenon. J Neurol 256:1236–1242. https://www.ncbi.nlm.nih.gov/pubmed/19306035
Haverkamp LJ, Appel V, Appel SH (1995) Natural history of amyotrophic lateral sclerosis in a database population. Brain 118:707–719. https://brain.oxfordjournals.org/content/brain/118/3/707.full.pdf
Turner MR, Goldacre R, Talbot K, Goldacre MJ (2016) Cerebrovascular injury as a risk factor for amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 87:244–246
Rosenbohm A, Kassubek J, Weydt P et al (2014) Can lesions to the motor cortex induce amyotrophic lateral sclerosis? J Neurol 261:283–290
Sivandzade F, Bhalerao A, Cucullo L (2019) Cerebrovascular and Neurological Disorders: Protective Role of NRF2. Int J Mol Sci 20:3433
Kahl A, Blanco I, Jackman K et al (2018) Cerebral ischemia induces the aggregation of proteins linked to neurodegenerative diseases. Sci Rep 8:2701. https://www.ncbi.nlm.nih.gov/pubmed/29426953
Mandrioli J, Ferri L, Fasano A et al (2018) Cardiovascular diseases may play a negative role in the prognosis of amyotrophic lateral sclerosis. Eur J Neurol 25:861–868
D’Amico E, Factir-Litvak P, Santella RM, Mitsumoto H (2013) Clinical perspective of oxidative stress in sporadic ALS. Free Radic Biol Med 29:997–1003
Roos E, Mariosa D, Ingre C et al (2016) Depression in amyotrophic lateral sclerosis. Neurology 86:2271–2277
Körner S, Kollewe K, Abdulla S, Zapf A, Dengler R, Petri S (2015) Interaction of physical function, quality of life and depression in amyotrophic lateral sclerosis: Characterization of a large patient cohort. BMC Neurol 2015:15
Lulé D, Häcker S, Ludolph A, Birbaumer N, Kübler A (2008) Depression and quality of life in patients with amyotrophic lateral sclerosis. Dtsch Arztebl Int 105:397–403. https://www.ncbi.nlm.nih.gov/pubmed/19626161
Rabkin JG, Albert SM, Del Bene ML et al (2005) Prevalence of depressive disorders and change over time in late-stage ALS. Neurology 65:62–67
Moore MJ, Moore PB, Shaw PJ (1998) Mood disturbances in motor neurone disease. J Neurol Sci 160(Suppl 1):S53–S56. https://www.ncbi.nlm.nih.gov/pubmed/9851650
Verschueren A, Kianimehr G, Belingher C et al (2019) Wish to die and reasons for living among patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Front Degener 20:68–73
Paganoni S, McDonnell E, Schoenfeld D et al (2017) Functional decline is associated with hopelessness in amyotrophic lateral sclerosis (ALS). J Neurol Neurophysiol. https://doi.org/10.4172/2155-9562.1000423
Il CC, Lee YD, Gwag BJ, Cho SI, Kim SS, Suh-Kim H (2008) Effects of estrogen on lifespan and motor functions in female hSOD1 G93A transgenic mice. J Neurol Sci 268:40–47
Groeneveld GJ, Van Muiswinkel FL, Sturkenboom JM, Wokke JHJ, Bär PR, Van Den Berg LH (2004) Ovariectomy and 17β-estradiol modulate disease progression of a mouse model of ALS. Brain Res 1021:128–131
Heitzer M, Kaiser S, Kanagaratnam M et al (2017) Administration of 17β-estradiol improves motoneuron survival and down-regulates inflammasome activation in male SOD1(G93A) ALS mice. Mol Neurobiol 54:8429–8443. https://www.ncbi.nlm.nih.gov/pubmed/27957680
Veldink JH, Sommer H, Weber M et al (2018) Prognosis for patients with amyotrophic lateral sclerosis: development and validation of a personalised prediction model. Lancet Neurol 17:423–433
Mandrioli J, Malerba SA, Beghi E et al (2018) Riluzole and other prognostic factors in ALS: a population-based registry study in Italy. J Neurol 265:817–827
Zoccolella S, Beghi E, Palagano G et al (2008) Analysis of survival and prognostic factors in amyotrophic lateral sclerosis: a population based study. J Neurol Neurosurg Psychiatry 79:33–37
Acknowledgements
The study was funded by the EU (ONWebDUALS project, JNPD 01ED1511B). We thank all project members and contributors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they do not have any conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Diekmann, K., Kuzma-Kozakiewicz, M., Piotrkiewicz, M. et al. Impact of comorbidities and co-medication on disease onset and progression in a large German ALS patient group. J Neurol 267, 2130–2141 (2020). https://doi.org/10.1007/s00415-020-09799-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09799-z