Abstract
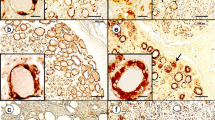
Ferritinopathy (neuroferritinopathy) has recently been identified as an autosomal dominant, multisystem disease, mainly affecting the central nervous system. It is caused by mutations in exon 4 of the ferritin light chain gene on chromosome 19. Its fine structural hallmarks are granular nuclear inclusions in neurons, oligodendroglial and microglial cells with similar extracellular derivatives in the central nervous system, muscle, peripheral nerve, and skin. These pathognostic structures have previously been described in perivascular cells of muscle and nerve biopsy specimens in a case with an obviously identical disease, formerly described as ‘granular nuclear inclusion body disease’. The nuclear inclusions, at the light microscopic level, are iron positive following histochemical iron reactions and immunoreactive for ferritin antibodies. At the electron microscopic level, in contrast to filamentous nuclear inclusions in ‘neuronal intranuclear hyaline inclusion disease’, dominant spinocerebellar atrophies and other trinucleotide repeat diseases, they are basically composed of granules measuring 5–15 nm. A moderate peak of iron detectable by energy dispersive microanalysis of the granular nuclear inclusions in ferritinopathy may also be significant. It is emphasized that ferritinopathy or ‘granular nuclear inclusion body disease’ can be diagnosed by a simple muscle or nerve biopsy without brain biopsy, autopsy, or molecular genetic testing of the considerable number of neurodegenerative diseases with possibly similar symptomatology.




Similar content being viewed by others
References
Abele M, Burk K, Andres F, Topka H, Laccone F, Bosch S, Brice A, Cancel G, Dichgans J, Klockgether T (1997) Autosomal dominant cerebellar ataxia type I. Nerve conduction and evoked potential studies in families with SCA1, SCA2 and SCA3. Brain 120:2141–2148
Bradley JL, Blake JC, Chamberlain S, Thomas PK, Cooper JM, Schapira AH (2000) Clinical, biochemical and molecular genetic correlations in Friedreich’s ataxia. Hum Mol Genet 9:275–282
Brulin P, Godfraind C, Leteurtre E, Ruchoux MM (2002) Morphometric analysis of ultrastructural vascular changes in CADASIL: analysis of 50 skin biopsy specimens and pathogenic implications. Acta Neuropathol 104:241–248
Castellani RJ, Siedlak SL, Perry G, Smith MA (2000) Sequestration of iron by Lewy bodies in Parkinson’s disease. Acta Neuropathol 100:111–114
Crompton DE, Chinnery PF, Fey C, Curtis AR, Morris CM, Kierstan J, Burt A, Young F, Coulthard A, Curtis A, Ince PG, Bates D, Jackson MJ, Burn J (2002) Neuroferritinopathy: a window on the role of iron in neurodegeneration. Blood Cells Mol Dis 29:522–531
Curtis AR, Fey C, Morris CM, Bindoff LA, Ince PG, Chinnery PF, Coulthard A, Jackson MJ, Jackson AP, McHale DP, Hay D, Barker WA, Markham AF, Bates D, Curtis A, Burn J (2001) Mutation in the gene encoding ferritin light polypeptide causes dominant adult-onset basal ganglia disease. Nat Genet 28:350–354
Jellinger KA (1999) The role of iron in neurodegeneration: prospects for pharmacotherapy of Parkinson’s disease. Drugs Aging 14:115–140
Jellinger KA (2002) Disturbance of the nigro-amygdaloid connections in dementia with Lewy bodies. J Neurol Sci 193:157–158
Jellinger KA (2003) How valid is the clinical diagnosis of Parkinson’s disease in the community? J Neurol Neurosurg Psychiatry 74:1005–1006
Kienzl E, Jellinger K, Stachelberger H, Linert W (1999) Iron as catalyst for oxidative stress in the pathogenesis of Parkinson’s disease? Life Sci 65:1973–1976
Lindenberg R, Rubinstein LJ, Herman MM, Haydon GB (1968) A light and electron microscopy study of an unusual widespread nuclear inclusion body disease. A possible residuum of an old herpesvirus infection. Acta Neuropathol (Berl) 10:54–73
Lowe JS, Leigh N (2002) Disorders of movement and system disorders. In: Graham DI, Lantos PL (eds) Greenfield’s neuropathology. Arnold, London, pp 325–430
Paulson HL, Perez MK, Trottier Y, Trojanowski JQ, Subramony SH, Das SS, Vig P, Mandel JL, Fischbeck KH, Pittman RN (1997) Intranuclear inclusions of expanded polyglutamine protein in spinocerebellar ataxia type 3. Neuron 19:333–344
Ruchoux MM, Guerouaou D, Vandenhaute B, Pruvo JP, Vermersch P, Leys D (1995) Systemic vascular smooth muscle cell impairment in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Acta Neuropathol 89:500–512
Schröder JM (1982) Pathologie der Muskulatur. In: Doerr W, Seifert G (eds) Spezielle pathologische Anatomie, vol 15. Springer, Berlin Heidelberg NewYork, pp 658–663
Schröder JM, Krämer KG, Hopf HC (1985) Granular nuclear inclusion body disease: fine structure of tibial muscle and sural nerve. Muscle Nerve 8:52–59
Schröder JM, Sellhaus B, Jörg J (1995) Identification of the characteristic vascular changes in a sural nerve biopsy of a case with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). Acta Neuropathol 89:116–121
Sung JH (1980) Light, fluorescence, and electron microscopic features of neuronal intranuclear hyaline inclusions associated with multisystem atrophy. Acta Neuropathol (Berl) 50:115–120
Sung JH, Ramirez-Lassepas M, Mastri AR, Larkin SM (1980) An unusual degenerative disorder of neurons associated with a novel intranuclear hyaline inclusion (neuronal intranuclear hyaline inclusion disease). A clinicopathological study of a case. J Neuropathol Exp Neurol 39:107–130
Takahashi Y, Miyajima H, Shirabe S, Nagataki S, Suenaga A, Gitlin JD (1996) Characterization of a nonsense mutation in the ceruloplasmin gene resulting in diabetes and neurodegenerative disease. Hum Mol Genet 5:81–84
Vidal R, Delisle MB, Rascol O, Ghetti B (2003) Hereditary ferritinopathy. J Neurol Sci 207:110–111
Vidal R, Ghetti B, Takao M, Brefel-Courbon C, Uro-Coste E, Glazier BS, Siani V, Benson MD, Calvas P, Miravalle L, Rascol O, Delisle MB (2004) Intracellular ferritin accumulation in neural and extraneural tissue characterizes a neurodegenerative disease associated with a mutation in the ferritin light polypeptide gene. J Neuropathol Exp Neurol 63:363–380
Author information
Authors and Affiliations
Corresponding author
Additional information
Dedicated to Prof. Kurt Jellinger on the occasion of his retirement as Managing Editor of Acta Neuropathologica
Rights and permissions
About this article
Cite this article
Schröder, J.M. Ferritinopathy: diagnosis by muscle or nerve biopsy, with a note on other nuclear inclusion body diseases. Acta Neuropathol 109, 109–114 (2005). https://doi.org/10.1007/s00401-004-0949-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-004-0949-5