Abstract
Background
The National Comprehensive Cancer Network (NCCN) guidelines recommend examination of a minimum of 12 lymph nodes (LNs) for accurate staging of a single case of colorectal cancer. However, the guidelines do not support the examination of LNs in synchronous colorectal carcinoma (SCC). This study aimed to investigate the association between lymph node yield and the prognosis of SCC patients.
Methods
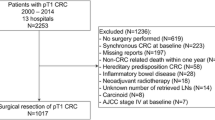
Synchronous colorectal carcinoma patients were selected from the Surveillance, Epidemiology, and End Results (SEER) database over a 10-year interval (2004 to 2013). Systematic dichotomization for optimal cut-off point identification was performed using X-tile. The baseline for the two LNs groups generated was balanced using the propensity score matching (PSM) method.
Results
A total of 4616 patients met the inclusion criteria. The cut-off number for lymph node retrieved from a single patient was 15 and 12 for the first- and second-time diagnosis of SCC, respectively. Age, T category, N category, tumor grade, tumor site, tumor size, and radiation sequence were not balanced in the two groups. After adjusting the baseline in the two groups, the same results were observed. Age, T category, N category, tumor site had a partial effect on lymph node yield. There might be some biological characteristics of the tumor that influence lymph node yield.
Conclusions
Retrieval of fewer than 15 LNs at the first time of SCC diagnosis indicates worse SCC prognosis. Because factors such as manner of surgical examination influence SCC prognosis, specimens should be preserved for at least 6 months to enable reevaluation should there be a need.
Irb: IRB approval is not required because the SEER data are freely accessible.





Similar content being viewed by others
Availability of data and materials
The datasets are available in SEER database to select the eligible cases. The data are also available from the corresponding author.
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30
Huang YQ, Liang CH, He L, Tian J, Liang CS, Chen X, Ma ZL, Liu ZY (2016) Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol 34(18):2157–2164
Hu H, Chang DT, Nikiforova MN, Kuan SF, Pai RK (2013) Clinicopathologic features of synchronous colorectal carcinoma: a distinct subset arising from multiple sessile serrated adenomas and associated with high levels of microsatellite instability and favorable prognosis. Am J Surg Pathol 37(11):1660–1670
Brandariz L, Alegre C, Rueda D, Arriba M, Alonso L, Nutu A, Rodríguez Y, Pajares JA, Ferrero E, García-Borda J, Perea J (2016) New perspectives in multiple primary colorectal cancer: a surgical approach. Digestion 94(2):57–65
Leersum NJ (2014) Van, Aalbers AG, Snijders HS, et al. Synchronous colorectal carcinoma: a risk factor in colorectal cancer surgery. Dis Colon Rectum 57(4):460–466
Joseph NE, Sigurdson ER, Hanlon AL, et al. Accuracy of determining nodal negativity in colorectal cancer on the basis of the number of nodes retrieved on resection. 2003.
Le Voyer TE, Sigurdson ER, Hanlon AL et al (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21(15):2912–2919
Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. 2003.
Tepper JE, O'Connell MJ, Niedzwiecki D et al (2001) Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 19(1):157–163
Sarli L, Bader G, Iusco D et al (2005) Number of lymph nodes examined and prognosis of TNM stage II colorectal cancer. Eur J Cancer (Oxford, England : 1990) 41(2):272–279
Johnson PM, Porter GA, Ricciardi R, Baxter NN (2006) Increasing negative lymph node count is independently associated with improved long-term survival in stage IIIB and IIIC colon cancer. J Clin Oncol 24(22):3570–3575
National Cancer Institute. Surveillance E, and End Results (SEER) Program. SEER*Stat Database: Incidence, SEER 18 Regs Public-Use (2015) Sub (1973–2013 varying), Linked To County Attributes, Total US, 1969–2014 Counties,National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch. [accessed 2018]: http://www.seer.cancer.gov/
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clinical cancer research : an official journal of the American Association for Cancer Research 10(21):7252–7259
Dai U, Akiyama G, Sugihara T, Magishi A, Yamaguchi T, Sano T (2017) Laparoscopic radical lymph node dissection for advanced colon cancer close to the hepatic flexure. Asian J Endosc Surg:10(1)
Lonjon G, Porcher R, Ergina P, Fouet M, Boutron I (2017) Potential pitfalls of reporting and bias in observational studies with propensity score analysis assessing a surgical procedure: a methodological systematic review. Ann Surg 265(5):901–909
Sauerbrei W, Royston P, Binder H (2007) Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med 26(30):5512–5528
Tibshirani R (1997) The lasso method for variable selection in the Cox model. Stat Med 16(4):385–395
Tibshirani R (2011) Regression shrinkage selection via the LASSO. J R Stat Soc Ser B Methodol 73:273–282
Benson AB, Venook AP, Al-Hawary MM et al (2018) NCCN Guidelines insights: colon cancer, Version 2.2018. J Natl Comp Cancer Netw : JNCCN 16(4):359–369
Benson AB, Venook AP, Al-Hawary MM et al (2018) Rectal Cancer, Version 2.2018, NCCN Clinical practice guidelines in oncology. J Natl Comp Cancer Netw : JNCCN 16(7):874–901
Dodgion CM, Neville BA, Lipsitz SR et al (2014) Hospital variation in sphincter preservation for elderly rectal cancer patients. J Surg Res 191(1):161–168
Morris AM, Billingsley KG, Baxter NN, Baldwin LM (2004) Racial disparities in rectal cancer treatment: a population-based analysis. Arch Surg (Chicago, Ill : 1960) 139(2):151–155 discussion 6
Massarweh NN, Hu CY, You YN et al (2014) Risk-adjusted pathologic margin positivity rate as a quality indicator in rectal cancer surgery. J Clin Oncol 32(27):2967–2974
Canessa CE, Badía F, Fierro S, Fiol V, Háyek G. Anatomic study of the lymph nodes of the mesorectum. 2001.
Topor B, Acland R, Kolodko V, Galandiuk S (2003) Mesorectal lymph nodes: their location and distribution within the mesorectum. Dis Colon Rectum 46(6):779–785
Goldstein NS (2002) Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years: recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am J Surg Pathol 26(2):179–189
Elferink MA, Siesling S, Lemmens VE et al (2011) Variation in lymph node evaluation in rectal cancer: a Dutch nationwide population-based study. Ann Surg Oncol 18(2):386–395
Pocard M, Panis Y, Malassagne B, Nemeth J, Hautefeuille P, Valleur P (1998) Assessing the effectiveness of mesorectal excision in rectal cancer: prognostic value of the number of lymph nodes found in resected specimens. Dis Colon Rectum 41(7):839–845
Goldstein NS (2002) Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years: recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am J Surg Pathol 26(2):179–189
Caplin S, Cerottini JP, Bosman FT, Constanda MT, Givel JC (1998) For patients with Dukes B (TNM Stage II) colorectal carcinoma, examination of six or fewer lymph nodes is related to poor prognosis. Cancer 83(4):666–672
Collette L, Bosset JF, den Dulk M et al (2007) Patients with curative resection of cT3-4 rectal cancer after preoperative radiotherapy or radiochemotherapy: does anybody benefit from adjuvant fluorouracil-based chemotherapy? A trial of the European Organisation for Research and Treatment of Cancer Radiation Oncology Group. J Clin Oncol 25(28):4379–4386
Khrizman P, Niland JC, ter Veer A et al (2013) Postoperative adjuvant chemotherapy use in patients with stage II/III rectal cancer treated with neoadjuvant therapy: a national comprehensive cancer network analysis. J Clin Oncol 31(1):30–38
You KY, Huang R, Ding PR, Qiu B, Zhou GQ, Chang H, Xiao WW, Zeng ZF, Pan ZZ, Gao YH (2014) Selective use of adjuvant chemotherapy for rectal cancer patients with ypN0. Int J Color Dis 29(4):529–538
Acknowledgments
We thank all the staff in the Department of Colorectal Surgery of FMUUH and gratefully acknowledge the SEER database (established by the National Cancer Institute, USA).
Funding
This study was supported by National Clinical Key Specialty Construction Project (General Surgery) of China; Wu Jieping Medical Foundation (320.2710.1833).
Author information
Authors and Affiliations
Contributions
YuXin Xu processed the data and carried out computational simulations.
XiaoJie Wang, Ying Huang, DaoXiong Ye helped on data collections and analyses.
YuXin Xu, Pan Chi, XiaoJie Wang, Ying Huang, DaoXiong Ye analyzed the results.
YuXin Xu, Pan Chi, XiaoJie Wang drafted the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The datasets are selected in SEER database. Ethics approval and consent to participate are not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
All authors reviewed and approved the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Appendix 2
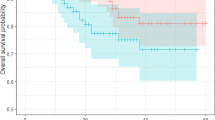
a and b indicate the optimal cut-off for differentiating between high- and low-risk LN groupings for the second time of SCC calculated by X-tile. c shows the optimal cut-off for distinguishing between high- and low-risk LN groupings for the second time of SCC diagnosis calculated by minimum p values.
Rights and permissions
About this article
Cite this article
Xu, Y., Huang, Y., Wang, X. et al. Prognostic significance of lymph node yield in patients with synchronous colorectal carcinomas. Int J Colorectal Dis 35, 2273–2282 (2020). https://doi.org/10.1007/s00384-020-03700-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03700-0