Abstract
Purpose
The use of intercostal nerve cryoablation (INC) is becoming increasingly common in patients undergoing pectus excavatum (PE) repair. This study sought to evaluate the use of INC compared to traditional use of thoracic epidural (TE).
Methods
A retrospective review of 79 patients undergoing PE repair with either INC or TE from May 2009 to December 2019 was conducted. The operations were performed by four surgeons who worked together at four different hospitals and have the same standardized practice. The primary outcome measure was hospital length of stay (LOS). Secondary variables included surgical time, total operating room time, operating room time cost, total hospital cost, inpatient opioid use, long-term opioid use after discharge, and postoperative complications.
Results
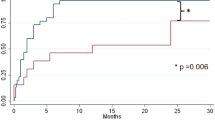
LOS decreased to 2.5 days in the INC group compared to 5 days in the TE group (p < 0.0001). Surgical time was increased in the INC group, but there was no difference in total OR time. The INC group experienced significantly lower hospital costs. Total hospital opioid administration was significantly lower in INC group, and there was a significant decrease in long-term opioid use in the INC group.
Conclusions
INC is a newer modality that decreases LOS, controls pain, and results in overall cost savings. We recommend that INC be included in the current practice for postoperative pain control in PE patients undergoing Nuss procedure.


Similar content being viewed by others
References
Fokin AA, Steuerwald NM, Ahrens WA, Allen KE (2009) Anatomical, histologic, and genetic characteristics of congenital chest wall deformities. Semin Thorac Cardiovasc Surg 21(1):44–57
Mao YZ, Tang S, Li S (2017) Comparison of the Nuss versus Ravitch procedure for pectus excavatum repair: an updated meta-analysis. J Pediatr Surg 52(10):1545–1552
Graves CE, Moyer J, Zobel MJ, Mora R, Smith D, O’Day M, Padilla BE (2019) Intraoperative intercostal nerve cryoablation during the Nuss procedure reduces length of stay and opioid requirement: a randomized clinical trial. J Pediatr Surg 54(11):2250–2256
Koh JC, Song Y, Kim SY, Park S, Ko SH, Han DW (2017) Postoperative pain and patient-controlled epidural analgesia-related adverse effects in young and elderly patients: a retrospective analysis of 2435 patients. J Pain Res 10:897–990
Stroud AM, Tulanont DD, Coates TE, Goodney PP, Croitoru DP (2014) Epidural analgesia versus intravenous patient-controlled analgesia following minimally invasive pectus excavatum repair: a systematic review and meta-analysis. J Pediatr Surg 49(5):798–806
St. Peter SD, Weesner KA, Weissend EE, Sharp SW, Valusek PA, Sharp RJ, Snyder CL, Holcomb GW, Ostlie DJ, (2012) Epidural vs patient-controlled analgesia for postoperative pain after pectus excavatum repair: a prospective, randomized trial. J Pediatr Surg 47(1):148–155
Lukosiene L, Rugyte DC, Macas A, Kalibatiene L, Malcius D, Barauskas V (2013) Postoperative pain management in pediatric patients undergoing minimally invasive repair of pectus excavatum: the role of intercostal block. J Pediatr Surg 48(12):2425–2430
Beltran R, Veneziano G, Bhalla T, Kenney B, Tumin D, Bissonnette B, Tobias JD (2017) Postoperative pain management in patients undergoing thoracoscopic repair of pectus excavatum: a retrospective analysis of opioid consumption and adverse effects in adolescents. Saudi J Anaesth 11(4):427
St Peter SD, Weesner KA, Sharp RJ, Sharp SW, Ostlie DJ, Holcomb GW (2008) Is epidural anesthesia truly the best pain management strategy after minimally invasive pectus excavatum repair? J Pediatr Surg 43(1):79–82
Litz CN, Farach SM, Fernandez AM, Elliott R, Dolan J, Nelson W, Walford NE, Snyder C, Jacobs JP, Amankwah EK, Danielson PD, Chandler NM (2017) Enhancing recovery after minimally invasive repair of pectus excavatum. Pediatr Surg Int 33(10):1123–1129
Man JY, Gurnaney HG, Dubow SR, DiMaggio TJ, Kroeplin GR, Adzick NS, Muhly WT (2017) A retrospective comparison of thoracic epidural infusion and multimodal analgesia protocol for pain management following the minimally invasive repair of pectus excavatum. Paediatr Anesth 27(12):1227–1234
Keller BA, Kabagambe SK, Becker JC, Chen YJ, Goodman LF, Clark-Wronski JM, Furukawa K, Stark RA, Rahm AL, Hirose S, Raff GW (2016) Intercostal nerve cryoablation versus thoracic epidural catheters for postoperative analgesia following pectus excavatum repair: preliminary outcomes in twenty-six cryoablation patients. J Pediatr Surg 51(12):2033–2038
US Centers for Medicare & Medicaid Services (2020) Opioid oral morphine milligram equivalent (MME) conversion factors. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Oral-MME-CFs-vFeb-2018.pdf. Accessed 19 Jun 2020
Nuss D, Obermeyer RJ, Kelly RE (2016) Nuss bar procedure: past, present and future. Ann Cardiothorac Surg 5(5):422
Loftus PD, Elder CT, Russell KW, Spanos SP, Barnhart DC, Scaife ER, Skarda DE, Rollins MD, Meyers RL (2016) Paravertebral regional blocks decrease length of stay following surgery for pectus excavatum in children. J Pediatr Surg 51(1):149–153
Melnick GA, Fonkych K (2016) Hospital prices increase in California, especially among hospitals in the largest multi-hospital systems. Inquiry 53:0046958016651555
Weissler EH, Sanati-Mehrizy P, Massenburg B, Jenny H, Taub PJ, Midulla PS (2016) Abstract complications, length of stay, and economic burden among children undergoing pectus excavatum repair. Plast Reconstr Surg Glob Open 4(9):198–199
Lloyd J, Barnard J, Glynn C (1976) Cryoanalgesia: a new approach to pain relief. Lancet 308(7992):932–934
Katz J, Nelson W, Forest R, Bruce D (1980) Cryoanalgesia for post-thoracotomy pain. Lancet 315(8167):512–513
Roberts D, Pizzarelli G, Lepore V, Al-Khaja N, Belboul A, Dernevik L (1988) Reduction of post-thoracotomy pain by cryotherapy of intercostal nerves. Scand J Thorac Cardiovasc Surg 22(2):127–130
Papic JC, Finnell SME, Howenstein AM, Breckler F, Leys CM (2014) Postoperative opioid analgesic use after Nuss versus Ravitch pectus excavatum repair. J Pediatr Surg 49(6):919–923
Hall Burton DM, Boretsky KR (2014) A comparison of paravertebral nerve block catheters and thoracic epidural catheters for postoperative analgesia following the Nuss procedure for pectus excavatum repair. Paediatr Anaesth 24(5):516–520
Graves C, Idowu O, Lee S, Padilla B, Kim S (2017) Intraoperative cryoanalgesia for managing pain after the Nuss procedure. J Pediatr Surg 52(6):920–924
Erinjeri JP, Clark TW (2010) Cryoablation: mechanism of action and devices. J Vasc Interv Radiol 21(8 Suppl):S187–S191
Zobel MJ, Ewbank C, Mora R, Idowu O, Kim S, Padilla BE (2020) The incidence of neuropathic pain after intercostal cryoablation during the Nuss procedure. Pediatr Surg Int 36(3):317–324
Author information
Authors and Affiliations
Contributions
RLR, AGR, HYL, DBS, AHC, and RMS conducted background research, conducted the study, and co-wrote/edited the manuscript. RLR and RMS also conducted the statistical analysis and interpreted the results.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rettig, R.L., Rudikoff, A.G., Lo, H.Y.A. et al. Cryoablation is associated with shorter length of stay and reduced opioid use in pectus excavatum repair. Pediatr Surg Int 37, 67–75 (2021). https://doi.org/10.1007/s00383-020-04778-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04778-x