Abstract
Background
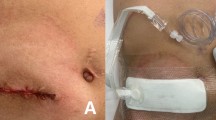
In neonatal surgical patients requiring an enterostomy, there is no definitive recommendation regarding the ideal enterostomy location: at the edge of the primary incision or at a different incision.
Methods
We retrospectively reviewed 2005–2017 administration data in our institution. All neonatal patients who underwent contaminated or dirty wound laparotomy and enterostomy construction were evaluated regarding the enterostomy location, occurrence of postoperative incisional surgical-site infection (SSI) at the primary incision, and stoma-related complications.
Results
Patients were divided into two groups based on stoma location: at the primary incision (the same incision group: SI group, n = 16) or at another incision (different incision group: DI group, n = 23). We performed 2 jejunostomies, 13 ileostomies, and 1 colostomy in the SI group, and 4 jejunostomies, 18 ileostomies, and 1 colostomy in the DI group. One of 16 patients (6.3%) in the SI group and 2/23 patients (8.7%) in the DI group experienced superficial incisional SSI, with comparable SSI incidence between groups (p = 0.78). Every SSI did not result in stoma-related complications.
Conclusions
Although the enterostomy location did not influence the incidence of laparotomy wound infection in this study, prospective studies are mandatory to fully assess the safety of enterostomy construction at the edge of the primary incision.
Similar content being viewed by others
References
Singh M, Owen A, Gull S et al (2006) Surgery for intestinal perforation in preterm neonates: anastomosis vs stoma. J Pediatr Surg 41:725–729
Haricharan RN, Gallimore JP, Nasr A (2017) Primary anastomosis or ostomy in necrotizing enterocolitis? Pediatr Surg Int 33:1139–1145
Bradnock TJ, Knight M, Kenny S et al (2017) British Association of Paediatric Surgeons Congenital Anomalies Surveillance System (BAPS-CASS). The use of stomas in the early management of Hirschsprung disease: findings of a national, prospective cohort study. J Pediatr Surg 52:1451–1457
Oda O, Davies D, Colapinto K et al (2014) Loop versus divided colostomy for the management of anorectal malformations. J Pediatr Surg 49:87–90
Garner JS (1986) CDC guideline for prevention of surgical wound infections, 1985. Supercedes guideline for prevention of surgical wound infections published in 1982. Revised Infect Control 7:193–200 (Originally published in 1995).
Horan TC, Gaynes RP, Martone WJ et al (1992) CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 13:606–608
Ricketts RR (1984) Surgical therapy for necrotizing enterocolitis. Ann Surg 200:653–657
Kronfli R, Maguire K, Walker GM (2013) Neonatal stomas: does a separate incision avoid complications and a full laparotomy at closure? Pediatr Surg Int 29:299–303
Segal I, Kang C, Albersheim SG et al (2014) Surgical site infections in infants admitted to the neonatal intensive care unit. J Pediatr Surg 49:381–384
Lejus C, Dumont R, Gall CL et al (2013) A preoperative stay in an intensive care unit is associated with an increased risk of surgical site infection in neonates. J Pediatr Surg 48:1503–1508
Vu LT, Vittinghoff E, Nobuhara KK et al (2014) Surgical site infections in neonates and infants: is antibiotic prophylaxis needed for longer than 24 h? Pediatr Surg Int 30:587–592
Clements KE, Fisher M, Quaye K et al (2016) Surgical site infections in the NICU. J Pediatr Surg 51:1405–1408
Acknowledgements
We thank Jane Charbonneau, DVM, and Angela Morben, DVM, from Edanz Group (http://www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Written informed consent was obtained from all of patients or guardians enrolled in this study.
Rights and permissions
About this article
Cite this article
Inoue, M., Uchida, K., Nagano, Y. et al. Impact of relationship between the stoma site and the primary incision on occurrence of laparotomy wound infection in contaminated or dirty wound operations in neonates. Pediatr Surg Int 34, 957–960 (2018). https://doi.org/10.1007/s00383-018-4310-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4310-9