Abstract
Purpose
Primary spontaneous pneumothorax (PSP) is managed in accordance with the adult British Thoracic Society (BTS) guidelines due to lack of paediatric evidence and consensus. We aim to highlight the differences and provide a best practice surgical management strategy for PSP based on experience of two major paediatric surgical centres.
Methods
Retrospective review of PSP management and outcomes from two UK Tertiary Paediatric hospitals between 2004 and 2015.
Results
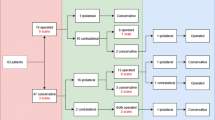
Fifty children with 55 PSP (5 bilateral) were referred to our Thoracic Surgical Services after initial management: 53 % of the needle aspirations failed. Nine children (20 %) were associated with visible bullae on the initial chest X-ray. Forty-nine children were assessed with computed tomography scan (CT). Apical emphysematous-like changes (ELC) were identified in 37 children (75 %). Ten children had also bullae in the asymptomatic contralateral lungs (20 %). In two children (4 %), CT demonstrated other lung lesions: a tumour of the left main bronchus in one child; a multi-cystic lesion of the right middle lobe in keeping with a congenital lung malformation in another child. Contralateral asymptomatic ELC were detected in 20 % of the children: of those 40 % developed pneumothorax within 6 months. Best surgical management was thoracoscopic staple bullectomy and pleurectomy with 11 % risk of recurrence. Histology confirmed ELC in 100 % of the apical lung wedge resections even in those apexes apparently normal at the time of thoracoscopy.
Conclusion
Our experience suggests that adult BTS guidelines are not applicable to children with large PSP. Needle aspiration is ineffective. We advocate early referral to a Paediatric Thoracic Service. We suggest early chest CT scan to identify ELC, for counselling regarding contralateral asymptomatic ELC and to rule out secondary pathological conditions causing pneumothorax. In rare instance if bulla is visible on presenting chest X-ray, thoracoscopy could be offered as primary option.


Similar content being viewed by others

References
Lesur O, Delorme N, Fromaget JM et al (1990) Computed tomography in the etiologic assessment of idiopathic spontaneous pneumothorax. Chest 98:341–347
Sahn SA, Heffner JE (2000) Spontaneous pneumothorax. N Engl J Med 342:868–874
Casali C, Stefani A, Ligabue G et al (2013) Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg 95:249–255
Martinez-Ramos D, Angel-Yepes V, Escrig-Sos J et al (2007) Usefulness of computed tomography in determining risk of recurrence after a first episode of primary spontaneous pneumothorax: therapeutic implications. Arch Bronconeumol 43:304–308
Noppen M, Dekeukeleire T, Hanon S et al (2006) Fluorescein-enhanced autofluorescence thoracoscopy in patients with primary spontaneous pneumothorax and normal subjects. Am J Respir Crit Care Med 174:26–30
Sihoe AD, Yim AP, Lee TW et al (2000) Can CT scanning be used to select patients with unilateral primary spontaneous pneumothorax for bilateral surgery? Chest 118:380–383
Huang TW, Lee SC, Cheng YL et al (2007) Contralateral recurrence of primary spontaneous pneumothorax. Chest 132:1146–1150
Noppen M, De Keukeleire T (2008) Pneumothorax. Respiration 76:121–127
Guimaraes CVA, Donnelly LF, Warner BW (2007) CT findings for blebs and bullae in children with spontaneous pneumothorax and comparison with findings in normal age-matched controls. Pediatr Radiol 37:879–884
BTS Pleural disease Guideline 2010. http://www.brit-thoracic.org.uk
Robinson PD, Blackburn C, Babl FE, on behalf of the Paediatric Emergency Departments International Collaborative (PREDICT) Research Network et al (2015) Management of paediatric spontaneous pneumothorax: a multicentre retrospective case series. Arch Dis Child. doi:10.1136/archdischild-2014-306696
Loeys BL, Dietz HC, Braverman AC et al (2010) The revised Ghent nosology for the Marfan syndrome. J Med Genet 47:476–485
Balbir-Gurman A, Guralnik L, Best LA et al (2009) Accelerated pulmonary nodulosis and sterile pleural effusion in a patient with psoriatic arthropathy during methotrexate therapy: a case report. J Clin Rheumatol 15:29–30
Seguier-Lipszyc E, Elizur A, Klin B et al (2011) Management of primary spontaneous pneumothorax in children. Clin Pediatr (Phila) 50:797–802
Nathan N, Guilbert J, Larroquet M et al (2010) Efficacy of blebs detection for preventive surgery in children’s idiopathic spontaneous pneumothorax. World J Surg 34:185–189
Choudhary AK, Sellars ME, Wallis C et al (2005) Primary spontaneous pneumothorax in children: the role of CT in guiding management. Clin Radiol 60:508–511
Shaw KS, Prasil P, Nguyen LT et al (2003) Pediatric spontaneous pneumothorax. Semin Pediatr Surg 12:55–61
Dines DE, Cortese DA, Brennan MD et al (1973) Malignant pulmonary neoplasms predisposing to spontaneous pneumothorax. Mayo Clin Proc 48:541–544
Escuissato DL, Adam GP, Urban LA et al (2003) Spontaneous bilateral pneumothoraces associated with Wilms tumor metastases. Pediatr Radiol 33:588–589
Laberge JM, Bratu I, Flageole H (2004) The management of asymptomatic congenital lung malformations. Pediatr Respir Rev 5 suppl A:S305–S312
Wong A, Vieten D, Singh S et al (2009) Long-term outcome of asymptomatic patients with congenital cystic adenomatoid malformation. Pediatr Surg Int 25:479–485
Sukki Cho, Ryu K, Jheon S et al (2009) Additional mechanical pleurodesis after thoracoscopic wedge resection and covering procedure for primary spontaneous pneumothorax. Surg Endosc 23:986–990
Körner H, Anderson KS, Stangeland L et al (1996) Surgical treatment of spontaneous pneumothorax by wedge resection without pleurodesis or pleurectomy. Eur J Cardiothorac Surg 10:656–659
Chung PH, Wong KK, Lan LC et al (2009) Thoracoscopic bullectomy for primary spontaneous pneumothorax in pediatric patients. Pediatr Surg Int 25:763–766
Horio H, Nomori H, Kobayashi R et al (2002) Impact of additional pleurodesis in video-assisted thoracoscopic bullectomy for primary spontaneous pneumothorax. Surg Endosc 16:630–634
Ayed AK, Al-Din HJ (2000) The results of thoracoscopic surgery for primary spontaneous pneumothorax. Chest 118:235–238
Chen JS, Hsu HH, Huang PM et al (2012) Thoracoscopic pleurodesis for primary spontaneous pneumothorax with high recurrence risk: a prospective randomized trial. Ann Surg 255:440–445
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soccorso, G., Anbarasan, R., Singh, M. et al. Management of large primary spontaneous pneumothorax in children: radiological guidance, surgical intervention and proposed guideline. Pediatr Surg Int 31, 1139–1144 (2015). https://doi.org/10.1007/s00383-015-3787-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3787-8