Abstract
Objective
To compare BI-RADS classification, management, and outcome of nonpalpable breast lesions assessed both by community practices and by a multidisciplinary tumor board (MTB) at a breast unit.
Methods
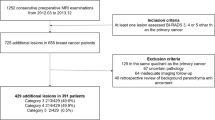
All nonpalpable lesions that were first assigned a BI-RADS score by community practices and then reassessed by an MTB at a single breast unit from 2009 to 2017 were retrospectively reviewed. Inter-review agreement was assessed with Cohen’s kappa statistic. Changes in biopsy recommendation were calculated. The percentage of additional tumor lesions detected by the MTB was obtained. The sensitivity, AUC, and cancer rates for BI-RADS category 3, 4, and 5 lesions were computed for both reviews.
Results
A total of 1909 nonpalpable lesions in 1732 patients were included. For BI-RADS scores in the whole cohort, a fair agreement was found (κ = 0.40 [0.36–0.45]) between the two reviews. Agreement was higher when considering only mammography combined with ultrasound (κ = 0.53 [0.44–0.62]), masses (κ = 0.50 [0.44–0.56]), and architectural distortion (κ = 0.44 [0.11–0.78]). Changes in biopsy recommendation occurred in 589 cases (31%). Ninety of 345 additional biopsies revealed high-risk or malignant lesions. Overall, the MTB identified 27% additional high-risk and malignant lesions compared to community practices. The BI-RADS classification AUCs for detecting malignant lesions were 0.66 (0.63–0.69) for community practices and 0.76 (0.75–0.78) for the MTB (p < 0.001).
Conclusion
Agreement between community practices and MTB reviews for BI-RADS classification in nonpalpable lesions is only fair. MTB review improves diagnostic performances of breast imaging and patient management.
Key Points
• The inter-review agreement for BI-RADS classification between community practices and the multidisciplinary board was only fair (κ = 0.40).
• Disagreements resulted in changes of biopsy recommendation in 31% of the lesions.
• The multidisciplinary board identified 27% additional high-risk and malignant lesions compared to community practices.




Similar content being viewed by others
Abbreviations
- MTB:
-
Multidisciplinary tumor board
- R1 BI-RADS:
-
BI-RADS score established by the community practice
- R1:
-
BI-RADS assessment by the community practice
- R2 BI-RADS:
-
BI-RADS score established by the multidisciplinary board at the breast unit
- R2:
-
BI-RADS assessment by the multidisciplinary board at the breast unit
References
American College of Radiology (ed) (1992) ACR BI-RADS® ATLAS, breast imaging reporting and data system, 1st edn. American College of Radiology, Reston
Lazarus E, Mainiero MB, Schepps B, Witt TR, Jokich P, Madrigrano A (2006) BI-RADS lexicon for US and mammography: interobserver variability and positive predictive value. Radiology 239:385–391. https://doi.org/10.1148/radiol.2392042127
Sickles EA, Wolverton DE, Dee KE (2002) Performance parameters for screening and diagnostic mammography: specialist and general radiologists. Radiology 224:861–869. https://doi.org/10.1148/radiol.2243011482
Chang JH, Vines E, Bertsch H et al (2001) The impact of a multidisciplinary breast cancer center on recommendations for patient management: the University of Pennsylvania experience. Cancer 91:1231–1237
Taylor C, Shewbridge A, Harris J, Green JS (2013) Benefits of multidisciplinary teamwork in the management of breast cancer. Breast Cancer (Dove Med Press) 5:79–85. https://doi.org/10.2147/BCTT.S35581
DiPiro PJ, vanSonnenberg E, Tumeh SS, Ros PR (2002) Volume and impact of second-opinion consultations by radiologists at a tertiary care cancer center: data. Acad Radiol 9:1430–1433
American College of Radiology (ed) (2003) ACR BI-RADS® ATLAS, breast imaging reporting and data system, 4th edn. American College of Radiology, Reston
American College of Radiology (ed) (2013) ACR BI-RADS® ATLAS, breast imaging reporting and data system, 5th edn. American College of Radiology, Reston
World Health Organization (2012) WHO classification of Tumours of the breast, 4th edn. World Health Organization, Geneva
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46. https://doi.org/10.1177/001316446002000104
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Spivey TL, Carlson KA, Janssen I, Witt TR, Jokich P, Madrigrano A (2015) Breast imaging second opinions impact surgical management. Ann Surg Oncol 22:2359–2364. https://doi.org/10.1245/s10434-014-4205-5
Pistolese CA, Lamacchia F, Tosti D et al (2020) Reducing the number of unnecessary percutaneous biopsies: the role of second opinion by expert breast center radiologists. Anticancer Res 40:939–950. https://doi.org/10.21873/anticanres.14027
Chang Sen LQ, Mayo RC, Lesslie MD, Yang WT, Leung JWT (2018) Impact of second-opinion interpretation of breast imaging studies in patients not currently diagnosed with breast Cancer. J Am Coll Radiol 15:980–987.e1. https://doi.org/10.1016/j.jacr.2018.03.055
Berg WA, Campassi C, Langenberg P, Sexton MJ (2000) Breast imaging reporting and data system: inter- and intraobserver variability in feature analysis and final assessment. AJR Am J Roentgenol 174:1769–1777
Lee AY, Wisner DJ, Aminololama-Shakeri S et al (2017) Inter-reader variability in the use of BI-RADS descriptors for suspicious findings on diagnostic mammography: a multi-institution study of 10 academic radiologists. Acad Radiol 24:60–66. https://doi.org/10.1016/j.acra.2016.09.010
Berg WA, D’Orsi CJ, Jackson VP et al (2002) Does training in the breast imaging reporting and data system (BI-RADS) improve biopsy recommendations or feature analysis agreement with experienced breast imagers at mammography? Radiology 224:871–880. https://doi.org/10.1148/radiol.2243011626
Timmers JMH, van Doorne-Nagtegaal HJ, Verbeek ALM, den Heeten GJ, Broeders MJM (2012) A dedicated BI-RADS training programme: effect on the inter-observer variation among screening radiologists. Eur J Radiol 81:2184–2188. https://doi.org/10.1016/j.ejrad.2011.07.011
Elmore JG, Jackson SL, Abraham L et al (2009) Variability in interpretive performance at screening mammography and radiologists’ characteristics associated with accuracy. Radiology 253:641–651. https://doi.org/10.1148/radiol.2533082308
Metzger-Filho O, Sun Z, Viale G et al (2013) Patterns of recurrence and outcome according to breast cancer subtypes in lymph node-negative disease: results from international breast cancer study group trials VIII and IX. J Clin Oncol 31:3083–3090. https://doi.org/10.1200/JCO.2012.46.1574
Barnard ME, Boeke CE, Tamimi RM (2015) Established breast cancer risk factors and risk of intrinsic tumor subtypes. Biochim Biophys Acta 1856:73–85. https://doi.org/10.1016/j.bbcan.2015.06.002
Collaborative Group on Hormonal Factors in Breast Cancer (2001) Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet 358:1389–1399. https://doi.org/10.1016/S0140-6736(01)06524-2
Brewer HR, Jones ME, Schoemaker MJ et al (2017) Family history and risk of breast cancer: an analysis accounting for family structure. Breast Cancer Res Treat 165:193–200. https://doi.org/10.1007/s10549-017-4325-2
Kesson EM, Allardice GM, George WD, Burns HJG, Morrison DS (2012) Effects of multidisciplinary team working on breast cancer survival: retrospective, comparative, interventional cohort study of 13 722 women. BMJ 344. https://doi.org/10.1136/bmj.e2718
Poma S, Longo A (2011) The clinician’s role in the diagnosis of breast disease. J Ultrasound 14:47–54. https://doi.org/10.1016/j.jus.2011.04.002
Coffey K, D’Alessio D, Keating DM, Morris EA (2017) Second-opinion review of breast imaging at a Cancer center: is it worthwhile? AJR Am J Roentgenol 208:1386–1391. https://doi.org/10.2214/AJR.16.16871
Newman EA, Guest AB, Helvie MA et al (2006) Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer 107:2346–2351. https://doi.org/10.1002/cncr.22266
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Cédric de Bazelaire.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (Axelle Dupont) has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
de Margerie-Mellon, C., Debry, JB., Dupont, A. et al. Nonpalpable breast lesions: impact of a second-opinion review at a breast unit on BI-RADS classification. Eur Radiol 31, 5913–5923 (2021). https://doi.org/10.1007/s00330-020-07664-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07664-1