Abstract
Objectives
Preoperative differentiation between benign lymphoepithelial lesion (BLEL) and mucosa-associated lymphoid tissue lymphoma (MALToma) in the parotid gland is important for treatment decisions. The purpose of this study was to develop and validate a CT-based radiomics nomogram combining radiomics signature and clinical factors for the preoperative differentiation of BLEL from MALToma in the parotid gland.
Methods
A total of 101 patients with BLEL (n = 46) or MALToma (n = 55) were divided into a training set (n = 70) and validation set (n = 31). Radiomics features were extracted from non-contrast CT images, a radiomics signature was constructed, and a radiomics score (Rad-score) was calculated. Demographics and CT findings were assessed to build a clinical factor model. A radiomics nomogram combining the Rad-score and independent clinical factors was constructed using multivariate logistic regression analysis. The performance levels of the nomogram, radiomics signature, and clinical model were evaluated and validated on the training and validation datasets, and then compared among the three models.
Results
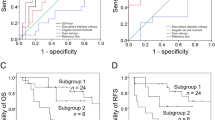
Seven features were used to build the radiomics signature. The radiomics nomogram incorporating the clinical factors and radiomics signature showed favorable predictive value for differentiating parotid BLEL from MALToma, with AUCs of 0.983 and 0.950 for the training set and validation set, respectively. Decision curve analysis showed that the nomogram outperformed the clinical factor model in terms of clinical usefulness.
Conclusions
The CT-based radiomics nomogram incorporating the Rad-score and clinical factors showed favorable predictive efficacy for differentiating BLEL from MALToma in the parotid gland, and may help in the clinical decision-making process.
Key Points
• Differential diagnosis between BLEL and MALToma in parotid gland is rather difficult by conventional imaging modalities.
• A radiomics nomogram integrated with the radiomics signature, demographics, and CT findings facilitates differentiation of BLEL from MALToma with improved diagnostic efficacy.






Similar content being viewed by others
Abbreviations
- 3-D:
-
Three-dimensional
- ANOVA:
-
Analysis of variance
- AUC:
-
Area under the curve
- BLEL:
-
Benign lymphoepithelial lesion
- CI:
-
Confidence interval
- DCA:
-
Decision curve analysis
- DCE:
-
Dynamic contrast-enhanced
- DWI:
-
Diffusion-weighted imaging
- GLCM:
-
Gray-level co-occurrence matrix
- GLDM:
-
Gray-level dependence matrix
- GLRLM:
-
Gray-level run length matrix
- GLSZM:
-
Gray-level size zone matrix
- ICC:
-
Inter-/intra- class correlation coefficient
- LASSO:
-
Least absolute shrinkage and selection operator
- MALT:
-
Mucosa-associated lymphoid tissue lymphoma
- NGTDM:
-
Neighboring gray tone difference matrix
- Nomo-score:
-
Nomogram score
- OR:
-
Odds ratio
- Rad-score:
-
Radiomics score
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
References
Aydin S, Demir MG, Barisik NO (2016) Extranodal marginal zone lymphoma of the parotid gland. J Maxillofac Oral Surg 15:346–350
Bende RJ, van Maldegem F, van Noesel CJ (2009) Chronic inflammatory disease, lymphoid tissue neogenesis and extranodal marginal zone B-cell lymphomas. Haematologica 94:1109–1123
Hwang JH, Kim DW, Kim KS, Lee SY (2019) Mucosa-associated lymphoid tissue lymphoma of the accessory parotid gland presenting as a simple cheek mass: a case report. Medicine (Baltimore) 98:e17042
Tagnon BB, Theate I, Weynand B, Hamoir M, Coche EE (2002) Long-standing mucosa-associated lymphoid tissue lymphoma of the parotid gland: CT and MR imaging findings. AJR Am J Roentgenol 178:1563–1565
DiGiuseppe JA, Corio RL, Westra WH (1996) Lymphoid infiltrates of the salivary glands: pathology, biology and clinical significance. Curr Opin Oncol 8:232–237
Sato K, Kawana M, Sato Y, Takahashi S (2002) Malignant lymphoma in the head and neck associated with benign lymphoepithelial lesion of the parotid gland. Auris Nasus Larynx 29:209–214
Zhu L, Wang P, Yang J, Yu Q (2013) Non-Hodgkin lymphoma involving the parotid gland: CT and MR imaging findings. Dentomaxillofac Radiol 42:20130046
Zhu L, Wang J, Shi H, Tao X (2019) Multimodality fMRI with perfusion, diffusion-weighted MRI and (1) H-MRS in the diagnosis of lympho-associated benign and malignant lesions of the parotid gland. J Magn Reson Imaging 49:423–432
Zhu L, Zhang C, Hua Y et al (2016) Dynamic contrast-enhanced MR in the diagnosis of lympho-associated benign and malignant lesions in the parotid gland. Dentomaxillofac Radiol 45:20150343
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures, they are data. Radiology 278:563–577
Buch K, Fujita A, Li B, Kawashima Y, Qureshi MM, Sakai O (2015) Using texture analysis to determine human papillomavirus status of oropharyngeal squamous cell carcinomas on CT. AJNR Am J Neuroradiol 36:1343–1348
Scalco E, Fiorino C, Cattaneo GM, Sanguineti G, Rizzo G (2013) Texture analysis for the assessment of structural changes in parotid glands induced by radiotherapy. Radiother Oncol 109:384–387
Sheikh K, Lee SH, Cheng Z et al (2019) Predicting acute radiation induced xerostomia in head and neck cancer using MR and CT radiomics of parotid and submandibular glands. Radiat Oncol 14:131
Pota M, Scalco E, Sanguineti G et al (2017) Early prediction of radiotherapy-induced parotid shrinkage and toxicity based on CT radiomics and fuzzy classification. Artif Intell Med 81:41–53
Alhamzawi R, Ali HTM (2018) The Bayesian adaptive lasso regression. Math Biosci 303:75–82
Wang T, Gao T, Guo H et al (2020) Preoperative prediction of parametrial invasion in early-stage cervical cancer with MRI-based radiomics nomogram. Eur Radiol. https://doi.org/10.1007/s00330-019-06655-1
Linden A (2006) Measuring diagnostic and predictive accuracy in disease management: an introduction to receiver operating characteristic (ROC) analysis. J Eval Clin Pract 12:132–139
Liu CC, Jethwa AR, Khariwala SS, Johnson J, Shin JJ (2016) Sensitivity, specificity, and posttest probability of parotid fine-needle aspiration: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 154:9–23
Schmidt RL, Hall BJ, Wilson AR, Layfield LJ (2011) A systematic review and meta-analysis of the diagnostic accuracy of fine-needle aspiration cytology for parotid gland lesions. Am J Clin Pathol 136:45–59
Epstein JB, Epstein JD, Le ND, Gorsky M (2001) Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92:519–525
Lieder A, Franzen A (2017) Management of primary malignant lymphoma of the parotid gland in a series of seven hundred and forty-five patients. Clin Otolaryngol 42:477–480
Maksimovic O, Bethge WA, Pintoffl JP et al (2008) Marginal zone B-cell non-Hodgkin’s lymphoma of mucosa-associated lymphoid tissue type: imaging findings. AJR Am J Roentgenol 191:921–930
Cantisani V, David E, De Virgilio A et al (2017) Prospective evaluation of quasistatic ultrasound elastography (USE) compared with baseline US for parotid gland lesions: preliminary results of elasticity contrast index (ECI) evaluation. Med Ultrason 19:32–38
Mansour N, Bas M, Stock KF, Strassen U, Hofauer B, Knopf A (2017) Multimodal ultrasonographic pathway of parotid gland lesions. Ultraschall Med 38:166–173
Altinbas NK, Gundogdu Anamurluoglu E, Oz II et al (2017) Real-time sonoelastography of parotid gland tumors. J Ultrasound Med 36:77–87
Zhang YF, Li H, Wang XM, Cai YF (2019) Sonoelastography for differential diagnosis between malignant and benign parotid lesions: a meta-analysis. Eur Radiol 29:725–735
Wong AJ, Kanwar A, Mohamed AS, Fuller CD (2016) Radiomics in head and neck cancer: from exploration to application. Transl Cancer Res 5:371–382
Scheckenbach K, Colter L, Wagenmann M (2017) Radiomics in head and neck cancer: extracting valuable information from data beyond recognition. ORL J Otorhinolaryngol Relat Spec 79:65–71
Al Ajmi E, Forghani B, Reinhold C, Bayat M, Forghani R (2018) Spectral multi-energy CT texture analysis with machine learning for tissue classification: an investigation using classification of benign parotid tumours as a testing paradigm. Eur Radiol 28:2604–2611
Fruehwald-Pallamar J, Czerny C, Holzer-Fruehwald L et al (2013) Texture-based and diffusion-weighted discrimination of parotid gland lesions on MR images at 3.0 Tesla. NMR Biomed 26:1372–1379
Fruehwald-Pallamar J, Hesselink JR, Mafee MF, Holzer-Fruehwald L, Czerny C, Mayerhoefer ME (2016) Texture-based analysis of 100 MR examinations of head and neck tumors - is it possible to discriminate between benign and malignant masses in a multicenter trial? Rofo 188:195–202
Wang Y, Liu W, Yu Y et al (2020) CT radiomics nomogram for the preoperative prediction of lymph node metastasis in gastric cancer. Eur Radiol 30:976–986
Zhao L, Gong J, Xi Y et al (2020) MRI-based radiomics nomogram may predict the response to induction chemotherapy and survival in locally advanced nasopharyngeal carcinoma. Eur Radiol 30:537–546
Hu T, Wang S, Huang L et al (2019) A clinical-radiomics nomogram for the preoperative prediction of lung metastasis in colorectal cancer patients with indeterminate pulmonary nodules. Eur Radiol 29:439–449
Tan X, Ma Z, Yan L, Ye W, Liu Z, Liang C (2019) Radiomics nomogram outperforms size criteria in discriminating lymph node metastasis in resectable esophageal squamous cell carcinoma. Eur Radiol 29:392–400
Acknowledgments
We thank Karl Embleton, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Da-peng Hao.
Conflict of interest
The authors declare that they have no conflict of interest.
Statistics and biometry
One of the authors (Da-peng Hao) has significant statistical expertise and is identified as the statistical guarantor for the statistical analysis used in this study.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study/observational/
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ying-mei Zheng as first author
Rights and permissions
About this article
Cite this article
Zheng, Ym., Xu, Wj., Hao, Dp. et al. A CT-based radiomics nomogram for differentiation of lympho-associated benign and malignant lesions of the parotid gland. Eur Radiol 31, 2886–2895 (2021). https://doi.org/10.1007/s00330-020-07421-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07421-4