Abstract
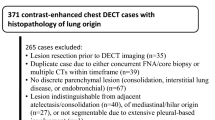
Objectives
To determine whether quantitative analysis of iodine-enhanced images generated from dual-energy CT (DECT) have added value in distinguishing invasive adenocarcinoma from non-invasive or minimally invasive adenocarcinoma (MIA) showing ground-glass nodule (GGN).
Methods
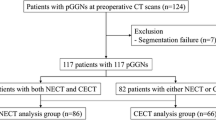
Thirty-four patients with 39 GGNs were enrolled in this prospective study and underwent DECT followed by complete tumour resection. Various quantitative imaging parameters were assessed, including virtual non-contrast (VNC) imaging and iodine-enhanced imaging.
Results
Of all 39 GGNs, four were adenocarcinoma in situ (AIS) (10 %), nine were MIA (23 %), and 26 were invasive adenocarcinoma (67 %). When assessing only VNC imaging, multivariate analysis revealed that mass, uniformity, and size-zone variability were independent predictors of invasive adenocarcinoma (odds ratio [OR] = 19.92, P = 0.02; OR = 0.70, P = 0.01; OR = 16.16, P = 0.04, respectively). After assessing iodine-enhanced imaging with VNC imaging, both mass on the VNC imaging and uniformity on the iodine-enhanced imaging were independent predictors of invasive adenocarcinoma (OR = 5.51, P = 0.04 and OR = 0.67, P < 0.01). The power of diagnosing invasive adenocarcinoma was improved after adding the iodine-enhanced imaging parameters versus VNC imaging alone, from 0.888 to 0.959, respectively (P = 0.029).
Conclusion
Quantitative analysis using iodine-enhanced imaging metrics versus VNC imaging metrics alone generated from DECT have added value in distinguishing invasive adenocarcinoma from AIS or MIA.
Key Points
• Quantitative analysis using DECT was used to distinguish invasive adenocarcinoma.
• Tumour mass and uniformity were independent predictors of invasive adenocarcinoma.
• Diagnostic performance was improved after adding iodine parameters to VNC parameters.






Similar content being viewed by others
Abbreviations
- AIS:
-
Adenocarcinoma in situ
- ATS:
-
American Thoracic Society
- AUC:
-
Area under the receiver operating characteristic curve
- CT:
-
Computed tomography
- DECT:
-
Dual-energy CT
- ERS:
-
European Respiratory Society
- GGN:
-
Ground-glass opacity nodule
- HU:
-
Hounsfield unit
- IASLC:
-
International Association for the Study of Lung Cancer
- MIA:
-
Minimally invasive adenocarcinoma
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- VNC:
-
Virtual non-contrast
References
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground-glass opacity lung nodules >/= 10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Son JY, Lee HY, Lee KS et al (2014) Quantitative CT analysis of pulmonary ground-glass opacity nodules for the distinction of invasive adenocarcinoma from pre-invasive or minimally invasive adenocarcinoma. PLoS One 9, e104066
Swensen SJ, Brown LR, Colby TV, Weaver AL (1995) Pulmonary nodules: CT evaluation of enhancement with iodinated contrast material. Radiology 194:393–398
Swensen SJ, Brown LR, Colby TV, Weaver AL, Midthun DE (1996) Lung nodule enhancement at CT: prospective findings. Radiology 201:447–455
Zhang M, Kono M (1997) Solitary pulmonary nodules: evaluation of blood flow patterns with dynamic CT. Radiology 205:471–478
Chae EJ, Song JW, Krauss B et al (2010) Dual-energy computed tomography characterization of solitary pulmonary nodules. J Thorac Imaging 25:301–310
Brooks RA (1977) A quantitative theory of the Hounsfield unit and its application to dual energy scanning. J Comput Assist Tomogr 1:487–493
Travis WD, Brambilla E, Noguchi M et al (2011) International association for the study of lung cancer/american thoracic society/european respiratory society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc 8:381–385
Naidich DP, Bankier AA, MacMahon H et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner society. Radiology 266:304–317
Chae EJ, Song JW, Seo JB, Krauss B, Jang YM, Song KS (2008) Clinical utility of dual-energy CT in the evaluation of solitary pulmonary nodules: initial experience. Radiology 249:671–681
Gupta R, Phan CM, Leidecker C et al (2010) Evaluation of dual-energy CT for differentiating intracerebral hemorrhage from iodinated contrast material staining. Radiology 257:205–211
de Hoop B, Gietema H, van de Vorst S, Murphy K, van Klaveren RJ, Prokop M (2010) Pulmonary ground-glass nodules: increase in mass as an early indicator of growth. Radiology 255:199–206
Mull RT (1984) Mass estimates by computed tomography: physical density from CT numbers. AJR Am J Roentgenol 143:1101–1104
Goh V, Ganeshan B, Nathan P, Juttla JK, Vinayan A, Miles KA (2011) Assessment of response to tyrosine kinase inhibitors in metastatic renal cell cancer: CT texture as a predictive biomarker. Radiology 261:165–171
Tixier F, Le Rest CC, Hatt M et al (2011) Intratumor heterogeneity characterized by textural features on baseline 18F-FDG PET images predicts response to concomitant radiochemotherapy in esophageal cancer. J Nucl Med 52:369–378
Chong Y, Kim JH, Lee HY et al (2014) Quantitative CT variables enabling response prediction in neoadjuvant therapy with EGFR-TKIs: are they different from those in neoadjuvant concurrent chemoradiotherapy? PLoS One 9, e88598
Ikeda K, Awai K, Mori T, Kawanaka K, Yamashita Y, Nomori H (2007) Differential diagnosis of ground-glass opacity nodules: CT number analysis by three-dimensional computerized quantification. Chest 132:984–990
Chandarana H, Rosenkrantz AB, Mussi TC et al (2012) Histogram analysis of whole-lesion enhancement in differentiating clear cell from papillary subtype of renal cell cancer. Radiology 265:790–798
Ozluk Y, Blanco PL, Mengel M, Solez K, Halloran PF, Sis B (2012) Superiority of virtual microscopy versus light microscopy in transplantation pathology. Clin Transpl 26:336–344
Travis WD, Brambilla E, Noguchi M et al (2011) International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
Kim HK, Choi YS, Kim J, Shim YM, Lee KS, Kim K (2010) Management of multiple pure ground-glass opacity lesions in patients with bronchioloalveolar carcinoma. J Thorac Oncol 5:206–210
Ganeshan B, Abaleke S, Young RC, Chatwin CR, Miles KA (2010) Texture analysis of non-small cell lung cancer on unenhanced computed tomography: initial evidence for a relationship with tumour glucose metabolism and stage. Cancer Imaging 10:137–143
Yi CA, Lee KS, Kim EA et al (2004) Solitary pulmonary nodules: dynamic enhanced multi-detector row CT study and comparison with vascular endothelial growth factor and microvessel density. Radiology 233:191–199
Weidner N, Semple JP, Welch WR, Folkman J (1991) Tumor angiogenesis and metastasis–correlation in invasive breast carcinoma. N Engl J Med 324:1–8
Swensen SJ, Morin RL, Schueler BA et al (1992) Solitary pulmonary nodule: CT evaluation of enhancement with iodinated contrast material–a preliminary report. Radiology 182:343–347
Yamashita K, Matsunobe S, Takahashi R et al (1995) Small peripheral lung carcinoma evaluated with incremental dynamic CT: radiologic-pathologic correlation. Radiology 196:401–408
Nelson DA, Tan TT, Rabson AB, Anderson D, Degenhardt K, White E (2004) Hypoxia and defective apoptosis drive genomic instability and tumorigenesis. Genes Dev 18:2095–2107
Thunnissen E, Beasley MB, Borczuk AC et al (2012) Reproducibility of histopathological subtypes and invasion in pulmonary adenocarcinoma. An international interobserver study. Mod Pathol 25:1574–1583
Kayser G, Kayser K (2013) Quantitative pathology in virtual microscopy: history, applications, perspectives. Acta Histochem 115:527–532
Neltner JH, Abner EL, Schmitt FA et al (2012) Digital pathology and image analysis for robust high-throughput quantitative assessment of Alzheimer disease neuropathologic changes. J Neuropathol Exp Neurol 71:1075–1085
Onozato ML, Klepeis VE, Yagi Y, Mino-Kenudson M (2012) A role of three-dimensional (3D) reconstruction in the classification of lung adenocarcinoma. Stud Health Technol Inform 179:250–256
Acknowledgments
The scientific guarantor of this publication is Ho Yun Lee. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding through grants from the Korean Foundation for Cancer Research (KFCR-CB-2011-02-02). Dr. Seonwoo Kim at the Biostatistics Unit of Samsung Biomedical Research Institute kindly provided statistical advice for this manuscript. Institutional Review Board approval was obtained (IRB 2011 09-083). Written informed consent was obtained from all patients in this study. Methodology: prospective, diagnostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Son, J.Y., Lee, H.Y., Kim, JH. et al. Quantitative CT analysis of pulmonary ground-glass opacity nodules for distinguishing invasive adenocarcinoma from non-invasive or minimally invasive adenocarcinoma: the added value of using iodine mapping. Eur Radiol 26, 43–54 (2016). https://doi.org/10.1007/s00330-015-3816-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3816-y