Abstract
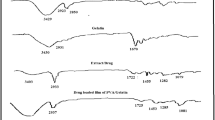
This study aims to develop procaine-loaded pectin hydrogels for both local anesthetic delivery and wound healing. We investigated the effects of initial drug concentration, pH of initial drug solution, and drying temperature of hydrogel on the drug release behavior of hydrogels. Fourier transform infrared spectroscopy, differential scanning calorimetry, and scanning electron microscopy were used for their characterization. Their swelling percentage, drug loading, and drug release behaviors were determined. Toxic effects of selected hydrogels on the wound healing ability of PCS-201-012 human dermal fibroblast cells and wound dressing properties were also investigated. According to our results, the hydrogels did not affect cell migration. Initial drug concentration, pH of initial drug solution, and drying temperature of hydrogels are crucial on procaine release behavior of pectin-based hydrogels.











Similar content being viewed by others
References
Bagshaw KR, Hanenbaum CL, Carbone EJ, Lo KW, Laurencin CT, Walker J, Nair LS (2015) Pain management via local anesthetics and responsive hydrogels. Ther Deliv 6:165–176. https://doi.org/10.4155/tde.14.95
Hirata K, Helal F, Hadgraft J, Lane ME (2013) Formulation of carbenoxolone for delivery to the skin. Int J Pharm 448:360–365. https://doi.org/10.1016/j.ijpharm.2013.03.045
Saxena P, Chandra A, Gupta S, Newaskar V (2013) Advances in dental local anesthesia techniques and devices: an update. Natl J Maxillofac Surg 4:19. https://doi.org/10.4103/0975-5950.117873
Hirata K, Mohammed D, Hadgraft J, Lane ME (2014) Influence of lidocaine hydrochloride and penetration enhancers on the barrier function of human skin. Int J Pharm 477:416–420. https://doi.org/10.1016/j.ijpharm.2014.10.012
Beiranvand S, Eatemadi A, Karimi A (2016) New updates pertaining to drug delivery of local anesthetics in particular bupivacaine using lipid nanoparticles. Nanoscale Res Lett 11:307. https://doi.org/10.1186/s11671-016-1520-8
Ustundag Okur N, Çağlar EŞ, Arpa MD, Karasulu Y (2017) Preparation and evaluation of novel microemulsion-based hydrogels for dermal delivery of benzocaine. Pharm Dev Technol 22:500–510. https://doi.org/10.3109/10837450.2015.1131716
Kurecic M, Maver T, Virant N, Ojstrsek A, Gradisnik L, Hribernik S, Kolar M, Maver U, Kleinschek KS (2018) A multifunctional electrospun and dual nano-carrier biobased system for simultaneous detection of pH in the wound bed and controlled release of benzocaine. Cellulose 25:7277–7297. https://doi.org/10.1007/s10570-018-2057-z
Morris T, Appleby R (1980) Retardation of wound healing by procaine. Br J Surg 67:391–392. https://doi.org/10.1002/bjs.1800670603
Chvapil M, Hameroff S, O'Dea K, Peacock EE (1979) Local anesthetics and wound healing. J Surg Res 27:367–371. https://doi.org/10.1016/0022-4804(79)90155-0
Wakamatsu T (1992) Effects of local anesthetics on healing process of extraction wound in rats with reference to effects of epinephrine, Kokubyo Gakkai zasshi. J Stomatol Soc Jpn 59:613–630
Rodrigues FV, Hochman B, Wood VT, Simões MJ, Juliano Y, Ferreira LM (2011) Effects of lidocaine with epinephrine or with buffer on wound healing in rat skin. Wound Repair Regener 19:223–228. https://doi.org/10.1111/j.1524-475X.2010.00654.x
Zeren S, Kesici S, Kesici U, Isbilir S, Turkmen UA, Ulusoy H, Karpuz V, Ozcan O, Polat E, Ipcioglu OM, Sari MK (2013) Effects of levobupivacaine on wound healing. Anesth Analg 116:495–499. https://doi.org/10.1213/ANE.0b013e318273f48e
Doǧan N, Üçok C, Korkmaz C, Üçok Ö, Karasu HA (2003) The effects of articaine hydrochloride on wound healing: an experimental study. J Oral Maxillofac Surg 61:1467–1470. https://doi.org/10.1016/j.joms.2003.05.002
Akcal A, Karsidag S, Yildiz K, Yesiloglu N, Akcal M, Kabukcuoglu F (2015) The effects of locally applied procaine on wound healing. Arch Clin Exp Surg 4:41–45. https://doi.org/10.5455/aces.20140606054447
Rezvanian M, Ahmad N, Amin MCIM, Ng SF (2017) Optimization, characterization, and in vitro assessment of alginate-pectin ionic cross-linked hydrogel film for wound dressing applications. Int J Biol Macromol 97:131–140. https://doi.org/10.1016/j.ijbiomac.2016.12.079
Johnson SM, Saint John BE, Dine AP (2008) Local anesthetics as antimicrobial agents: a review. Surg Infect (Larchmt) 9:205–213. https://doi.org/10.1089/sur.2007.036
Culp WC, Culp WC (2011) Practical application of local anesthetics. J Vasc Interv Radiol 22:111–118. https://doi.org/10.1016/j.jvir.2010.10.005
Maver T, Hribernik S, Mohan T, Smrke DM, Maver U, Stana-Kleinschek K (2015) Functional wound dressing materials with highly tunable drug release properties. RSC Adv 5:77873–77884. https://doi.org/10.1039/c5ra11972c
Xu K, Kleinbeck KR, Kao WJ (2012) Multifunctional biomaterial matrix for advanced wound healing. Adv Wound Care 1:75–80. https://doi.org/10.1089/wound.2011.0349
Ninan N, Muthiah M, Yahaya NAB, Park IK, Elain A, Wong TW, Thomas S, Grohens Y (2014) Antibacterial and wound healing analysis of gelatin/zeolite scaffolds. Colloids Surf B Biointerfaces 115:244–252. https://doi.org/10.1016/j.colsurfb.2013.11.048
Rampino A, Borgogna M, Bellich B, Blasi P, Virgilio F, Cesàro A (2016) Chitosan–pectin hybrid nanoparticles prepared by coating and blending techniques. Eur J Pharm Sci 84:37–45. https://doi.org/10.1016/j.ejps.2016.01.004
Neufeld L, Bianco-Peled H (2017) Pectin–chitosan physical hydrogels as potential drug delivery vehicles. Int J Biol Macromol 101:852–861. https://doi.org/10.1016/j.ijbiomac.2017.03.167
Munarin F, Tanzi MC, Petrini P (2012) Advances in biomedical applications of pectin gels. Int J Biol Macromol 51:681–689. https://doi.org/10.1016/j.ijbiomac.2012.07.002
Esposito M, DiPierro P, Regalado-Gonzales C, Mariniello L, Giosafatto CVL, Porta R (2016) Polyamines as new cationic plasticizers for pectin-based edible films. Carbohydr Polym 153:222–228. https://doi.org/10.1016/j.carbpol.2016.07.087
Güner OZ, Cam C, Arabacioglu-Kocaaga B, Batirel S, Güner FS (2018) Theophylline-loaded pectin-based hydrogels. I. Effect of medium pH and preparation conditions on drug release profile. J Appl Polym Sci 135:46731. https://doi.org/10.1002/APP.46731
Tan JP, Zeng AQ, Chang CC, Tam KC (2008) Release kinetics of procaine hydrochloride (PrHy) from pH-responsive nanogels: theory and experiments. Int J Pharm 357:305–313. https://doi.org/10.1016/j.ijpharm.2008.01.058
BS EN 12127:1998 (1998) Textiles fabrics determination of mass per unit area using small samples. British Standard Institute, London. ISBN 0-580-29132-4
BN EN ISO 9073-2:1997 (1997) Textiles, Test methods for nonwovens, part 2: determination of thickness. British Standard Institute, London
D522-93a, Standard test methods for mandrel bend test of attached organic coatings. American Society for Testing and Materials
D2240-97 standard test method for rubber property—durometer hardness. American Society for Testing and Materials
BS EN 13726-1:2002 (2002) Test methods for primary wound dressings. Aspect of absorbency, BSI. British Standard Institute, London. ISBN 0-580-39510-3
Parsons D, Bowler PG, Myles V, Jones S (2005) Silver antimicrobial dressings in wound management: a comparison of antibacterial, physical, and chemical characteristics. Wounds 17:222–232
BS EN 13726-2:2001 (2001) Test method for primary wound dressing. Part 1: aspect of absorbency, section 3.6, dispersion characteristics. British Standard Institute, London
ASTM E96 Standard Test Methods for water vapor transmission of materials. American Society for Testing and Materials
Du WX, Olsen CW, Avena-Bustillos RJ, McHugh TH, Levin CE, Mandrell R, Friedman M (2009) Antibacterial effects of allspice, garlic, and oregano essential oils in tomato films determined by overlay and vapor-phase methods. J Food Sci 74:M390–M397. https://doi.org/10.1111/j.1750-3841.2009.01289.x
Das B, Nayak AK, Nanda U (2013) Topical gels of lidocaine HCl using cashew gum and Carbopol 940: preparation and in vitro skin permeation. Int J Biol Macromol 62:514–517. https://doi.org/10.1016/j.ijbiomac.2013.09.049
Shin SC, Cho CW, Yang KH (2004) Development of lidocaine gels for enhanced local anesthetic action. Int J Pharm 287:73–78. https://doi.org/10.1016/j.ijpharm.2004.08.012
Latif IA, Abdullah HM, Saleem MH (2016) Electrical and swelling study of different prepared hydrogel. Am J Polym Sci 6:50–57. https://doi.org/10.5923/j.ajps.20160602.04
Mishra RK, Datt M, Banthia AK (2008) Synthesis and characterization of pectin/PVP hydrogel membranes for drug delivery system. AAPS Pharm Sci Technol 9:395–403. https://doi.org/10.1208/s12249-008-9048-6
Fuliaş A, Ledeţi I, Vlase G, Popoiu C, Hegheş A, Bilanin M, Vlase T, Gheorgheosu D, Craina M, Ardelean S, Ferechide D, Mǎrginean O, Moş L (2013) Thermal behaviour of procaine and benzocaine. Part II: compatibility study with some pharmaceutical excipients used in solid dosage forms. Chem Cent J 7:1–10. https://doi.org/10.1186/1752-153X-7-140
Pourjavadi A, Barzegar S (2009) Synthesis and evaluation of pH and thermosensitive pectin-based superabsorbent hydrogel for oral drug delivery systems. Starch/Staerke 61:161–172. https://doi.org/10.1002/star.200800063
Namazi H, Rakhshaei R, Hamishehkar H, Kafil HS (2016) Antibiotic loaded carboxy methyl cellulose/MCM-41 nanocomposite hydrogel films as potential wound dressing. Int J Biol Macromol 85:327–334. https://doi.org/10.1016/j.ijbiomac.2015.12.076
Opanasopit P, Apirakaramwong A, Ngawhirunpat T, Rojanarata T, Ruktanonchai U (2008) Development and characterization of pectinate micro/nanoparticles for gene delivery. AAPS Pharm Sci Technol 9:67–74. https://doi.org/10.1208/s12249-007-9007-7
Tan JP, Goh CH, Tam KC (2007) Comparative drug release studies of two cationic drugs from pH-responsive nanogels. Eur J Pharm Sci 32:340–348. https://doi.org/10.1016/j.ejps.2007.08.010
Samanta HS, Ray SK (2014) Controlled release of tinidazole and theophylline from chitosan based composite hydrogels. Carbohydr Polym 106:109–120. https://doi.org/10.1016/j.carbpol.2014.01.097
Sriamornsak P (1999) Effect of calcium concentration, hardening agent and drying condition on release characteristics of oral proteins from calcium pectinate gel beads. Eur J Pharm Sci 8:221–227. https://doi.org/10.1016/S0928-0987(99)00010-X
De Cicco F, Reverchon E, Adami R, Auriemma G, Russo P, Calabrese EC, Porta A, Aquino RP, Del Gaudio P (2014) In situ forming antibacterial dextran blend hydrogel for wound dressing: SAA technology vs. spray drying. Carbohydr Polym 101:1216–1224. https://doi.org/10.1016/j.carbpol.2013.10.067
Lin LS, Yuen HK, Varner JE (1991) Differential scanning calorimetry of plant cell walls. Proc Natl Acad Sci USA 88:2241–2243. https://doi.org/10.1073/pnas.88.6.2241
Physicochemical properties of drugs. In: Donald C (ed) Essentials of pharmaceutical chemistry (2012). Sample chapter copyright Pharmaceutical Press, pp 57–79. https://www.pharmpress.com/files/docs/EssentialsPharmaceuticalChemistry_Sample(2).pdf. Accessed 24 Dec 2018
Shilpa A, Agrawal SS, Ray AR (2003) Controlled delivery of drugs from alginate matrix. J Macromol Sci C Polym Rev 43(2):187–221. https://doi.org/10.1081/MC-12002016
Segi N, Yotsuyanagi T, Ikeda K (1989) Interaction of calcium-alginate gel beads with propranolol. Chem Pharm Bull 37(11):3092–3095. https://doi.org/10.1248/cpb.37.3092
You JO, Park SB, Park HY, Haam S, Chung CH, Kim WS (2001) Preparation of regular sized Ca-alginate microspheres using membrane emulsification method. J Microencapsul 18(4):521–532. https://doi.org/10.1248/cpb.37.3092
Zhila I, Adeleh D, Akbar AS, Sawyer L (2016) β-Lactoglobulin–pectin nanoparticle-based oral drug delivery system for potential treatment of colon cancer. Chem Biol Drug Des 88:209–216. https://doi.org/10.1111/cbdd.12748
Skorkowska-Telichowska K, Czemplik M, Kulma A, Szopa J (2013) The local treatment and available dressings designed for chronic wounds. J Am Acad Dermatol 68:e117. https://doi.org/10.1016/j.jaad.2011.06.028
Jantrawut P, Bunrueangtha J, Suerthong J (2019) Fabrication and characterization of low methoxyl pectin/gelatin/carboxymethyl cellulose absorbent hydrogel film for wound dressing applications. Materials 12:1628. https://doi.org/10.3390/ma12101628
Uzun M, Anand SC, Shah AT (2013) In vitro characterization and evaluation of different types of wound dressing materials. J Biomed Eng Technol 1(2013):1–7
Balakrishnan B, Mohanty M, Umashankar PR, Jayakrishnan A (2005) Evaluation of an in situ forming hydrogel wound dressing based on oxidized alginate and gelatin. Biomaterials 26:6335–6342. https://doi.org/10.1016/j.biomaterials.2005.04.012
Shahzad A, Khan A, Afzal Z, Umer MF, Khan J, Khan GM (2019) Formulation development and characterization of cefazolin nanoparticles-loaded cross-linked films of sodium alginate and pectin as wound dressings. Int J Biol Macromol 124:255–269. https://doi.org/10.1016/j.ijbiomac.2018.11.090
Rezvanian M, Ahmad N, Mohd Amin MCI, Ng SF (2017) Optimization, characterization, and in vitro assessment of alginate-pectin ionic cross-linked hydrogel film for wound dressing applications. Int J Biol Macromol 97:131–140. https://doi.org/10.1016/j.ijbiomac.2016.12.079
Alavi T, Rezvanian M, Ahmad N, Mohamad N, Ng SF (2019) Pluronic-F127 composite film loaded with erythromycin for wound application: formulation, physicomechanical and in vitro evaluations. Drug Deliv Transl Res 9:508–519. https://doi.org/10.1007/s13346-017-0450-z
Acknowledgements
We sincerely thank Herbstreith & Fox company for providing low-methylated pectin. This work was funded by The Scientific and Technological Research Council of Turkey (TUBITAK) with 115M439 of Project Number.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rodoplu, S., Celik, B.E., Kocaaga, B. et al. Dual effect of procaine-loaded pectin hydrogels: pain management and in vitro wound healing. Polym. Bull. 78, 2227–2250 (2021). https://doi.org/10.1007/s00289-020-03210-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-020-03210-7