Abstract
Purpose
This study evaluates baseline patient characteristics and surgical parameters for risk factors of medical complications in ASD patients received posterior long level internal fixation.
Methods
Analysis of consecutive patients who underwent posterior long-level instruction fixation for adult degenerative scoliosis (ADS) with a minimum of two year follow-up was performed. Pre-operative risk factors, intraoperative variables, peri-operative radiographic parameters, and surgical-related risk factors were collected to analyze the effect of risk factors on medical complications. Patients were separated into groups with and without medical complication. Then, complication group was further classified as major or minor medical complications. Potential risk factors were identified by univariate testing. Multivariate logistic regression was used to evaluate independent predictors of medical complications.
Results
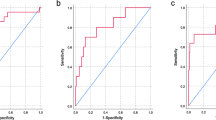
One hundred and thirty-one ADS patients who underwent posterior long segment pedicle screws fixation were included. Total medical complication incidence was 25.2%, which included infection (12.2%), neurological (11.5%), cardiopulmonary (7.6%), gastrointestinal (6.1%), and renal (1.5%) complications. Overall, 7.6% of patients developed major medical complications, and 17.6% of patients developed minor medical complications. The radiographic parameters of pre-operative and last follow-up had no significant difference between the groups of medical complications and the major or minor medical complications subgroups. However, the incidence of cerebrospinal fluid leak (CFL) in patients who without medical complications was much lower than that with medical complications (18.4 vs. 42.4%, P = 0.005). Independent risk factors for development of medical complications included smoking (OR = 6.45, P = 0.012), heart disease (OR = 10.07, P = 0.012), fusion level (OR = 2.12, P = 0.001), and length of hospital stay (LOS) (OR = 2.11, P = 0.000). Independent risk factors for development of major medical complications were diabetes (OR 6.81, P = 0.047) and heart disease (OR = 5.99, P = 0.049). Except for the last follow-up, Oswestry Disability Index and visual analog scale of the patient experienced medical complications trend higher score; the clinical outcomes have no significant difference between the medical and major complications groups.
Conclusion
Heart disease comorbidity is an independent risk factor for both medical and major medical complications. Smoking, fusion level, and LOS are independent risk factors for medical complication. Diabetes is the independent risk factors for major medical complications.
Similar content being viewed by others
References
Hawasli AH, Chang J, Yarbrough CK, Steger-May K, Lenke LG, Dorward IG (2016) Interpedicular height as a predictor of radicular pain in adult degenerative scoliosis. Spine J 16(9):1070–1078
Carter OD, Haynes SG (1987) Prevalence rates for scoliosis in US adults: results from the first National Health and nutrition examination survey. Int J Epidemiol 16(4):537–544
Birknes JK, White AP, Albert TJ, Shaffrey CI, Harrop JS (2008) Adult degenerative scoliosis: a review. Neurosurgery 63(3 Suppl):94–103
Grevitt M, Khazim R, Webb J, Mulholland R, Shepperd J (1997) The short form-36 health survey questionnaire in spine surgery. J Bone Joint Surg Br 79(1):48–52
Korovessis P, Piperos G, Sidiropoulos P, Dimas A (1994) Adult idiopathic lumbar scoliosis. A formula for prediction of progression and review of the literature. Spine (Phila Pa 1976) 19(17):1926–1932
Perdriolle R, Vidal J (1985) Thoracic idiopathic scoliosis curve evolution and prognosis. Spine (Phila Pa 1976) 10(9):785–791
Cho KJ, Kim YT, Shin SH, Suk SI (2014) Surgical treatment of adult degenerative scoliosis. Asian Spine J 8(3):371–381
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 34(17):1828–1833
Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL (2010) Natural history of spinopelvic alignment differs from symptomatic deformity of the spine. Spine (Phila Pa 1976) 35(16):E792–E798
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30(18):2024–2029
Hsieh M K, Chen L H, Niu C C, Fu T S, Lai P L, Chen W J (2015) Combined anterior lumbar interbody fusion and instrumented posterolateral fusion for degenerative lumbar scoliosis: indication and surgical outcomes. BMC Surg 15(15):26
Gurr KR, McAfee PC, Shih CM (1988) Biomechanical analysis of anterior and posterior instrumentation systems after corpectomy. A calf-spine model. J Bone Joint Surg 70(8):1182–1191
Nguyen HV, Akbarnia BA, van Dam BE, Raiszadeh K, Bagheri R, Canale S, Sylvain GM, Barone R, Bench G (2006) Anterior exposure of the spine for removal of lumbar interbody devices and implants. Spine (Phila Pa 1976) 31(21):2449–2453
Brau SA, Delamarter RB, Kropf MA, Watkins RG 3rd, Williams LA, Schiffman ML, Bae HW (2008) Access strategies for revision in anterior lumbar surgery. Spine (Phila Pa 1976) 33(15):1662–1667
Gumbs AA, Hanan S, Yue JJ, Shah RV, Sumpio B (2007) Revision open anterior approaches for spine procedures. Spine J 7(3):280–285
Park P, Wang MY, Lafage V, Nguyen S, Ziewacz J, Okonkwo DO, Uribe JS, Eastlack RK, Anand N, Haque R, Fessler RG, Kanter AS, Deviren V, La Marca F, Smith JS, Shaffrey CI, Mundis GM Jr, Mummaneni PV, International Spine Study Group (2015) Comparison of two minimally invasive surgery strategies to treat adult spinal deformity. J Neurosurg Spine 22(4):374–380
Crandall DG, Revella J (2009) Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine (Phila Pa 1976) 34(20):2126–2133
Zimmerman RM, Mohamed AS, Skolasky RL, Robinson MD, Kebaish KM (2010) Functional outcomes and complications after primary spinal surgery for scoliosis in adults aged forty years or older: a prospective study with minimum two-year follow-up. Spine (Phila Pa 1976) 35(20):1861–1866
Pichelmann MA, Lenke LG, Bridwell KH, Good CR, O'Leary PT, Sides BA (2010) Revision rates following primary adult spinal deformity surgery: six hundred forty-three consecutive patients followed-up to twenty-two years postoperative. Spine (Phila Pa 1976) 35(2):219–226
Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Lee TJ, Lee JJ, Lee JM (2008) Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J 17(5):650–656
Soroceanu A, Burton DC, Oren JH, Smith JS, Hostin R, Shaffrey CI, Akbarnia BA, Ames CP, Errico TJ, Bess S, Gupta MC, Deviren V, Schwab FJ, Lafage V, International Spine Study Group (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976) 41(22):1718–1723
Soroceanu A, Burton D C, Diebo B G, Smith J S, Hostin R, Shaffrey C I, Boachie-Adjei O, Mundis G M, Jr, Ames C, Errico T J, Bess S, Gupta M C, Hart R A, Schwab F J, Lafage V, International Spine Study Group (2015) Impact of obesity on complications, infection, and patient-reported outcomes in adult spinal deformity surgery. J Neurosurg Spine 1–9
Helgeson MD, Shah SA, Newton PO, Clements DH, Betz RR, Marks MC, Bastrom T (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35(2):177–181
Kim K-T, Lee S-H, Suk K-S, Lee J-H, Im Y-J (2007) Spinal pseudarthrosis in advanced ankylosing spondylitis with sagittal plane deformity. Spine 32(15):1641–1647
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32(24):2764–2770
Du J, Tang X, Li N, Zhang L, Zhang X (2016) Limited long-segment fusion for degenerative lower lumbar scoliosis: a special kind of scoliosis. Int Orthop 40(6):1227–1231
Bianco K, Norton R, Schwab F, Smith JS, Klineberg E, Obeid I, Mundis G Jr, Shaffrey CI, Kebaish K, Hostin R, Hart R, Gupta MC, Burton D, Ames C, Boachie-Adjei O, Protopsaltis TS, Lafage V, International Spine Study G (2014) Complications and intercenter variability of three-column osteotomies for spinal deformity surgery: a retrospective review of 423 patients. Neurosurg Focus 36(5):E18
Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, Crawford CH 3rd, O'Shaughnessy BA, Buchowski JM, Chang MS, Zebala LP, Sides BA (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 37(14):1198–1210
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976) 31(20):2329–2336
Yamato Y, Matsuyama Y, Hasegawa K, Aota Y, Akazawa T, Iida T, Ueyama K, Uno K, Kanemura T, Kawakami N, Kotani T, Takaso M, Takahashi J, Tanaka M, Taneichi H, Tsuji T, Hosoe H, Mochida J, Shimizu T, Yonezawa I, Watanabe K, Matsumoto M, Committee for Adult Deformity J S S (2017) A Japanese nationwide multicenter survey on perioperative complications of corrective fusion for elderly patients with adult spinal deformity. J Orthop Sci 22(2):237–242
Kothari P, Lee NJ, Leven DM, Lakomkin N, Shin JI, Skovrlj B, Steinberger J, Guzman JZ, Cho SK (2016) Impact of gender on 30-day complications after adult spinal deformity surgery. Spine (Phila Pa 1976) 41(14):1133–1138
Ou CY, Lee TC, Lee TH, Huang YH (2015) Impact of body mass index on adjacent segment disease after lumbar fusion for degenerative spine disease. Neurosurgery 76(4):396–401; discussion 401-392; quiz 402
Urban MK, Jules-Elysee KM, Beckman JB, Sivjee K, King T, Kelsey W, Boachie-Adjei O (2005) Pulmonary injury in patients undergoing complex spine surgery. Spine J 5(3):269–276
Kostuik JPHB (1983) Spinal fusions to the sacrum in adults with scoliosis. Spine (Phila Pa 1976) 8(5):489–500
Jin M, Liu Z, Qiu Y, Yan H, Han X, Zhu Z (2017) Incidence and risk factors for the misplacement of pedicle screws in scoliosis surgery assisted by O-arm navigation-analysis of a large series of one thousand, one hundred and forty five screws. Int Orthop 41(4):773–780
Cho SK, Bridwell KH, Lenke LG, Yi JS, Pahys JM, Zebala LP, Kang MM, Cho W, Baldus CR (2012) Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine (Phila Pa 1976) 37(6):489–500
Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D, Study Group on S (2012) Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976) 37(8):693–700
Blamoutier A, Guigui P, Charosky S, Roussouly P, Chopin D, Groupe d'Etude de la S (2012) Surgery of lumbar and thoracolumbar scolioses in adults over 50. Morbidity and survival in a multicenter retrospective cohort of 180 patients with a mean follow-up of 4.5 years. Orthop Traumatol Surg Res 98(5):528–535
Kim HJ, Iyer S, Zebala LP, Kelly MP, Sciubba D, Protopsaltis TS, Gupta M, Neuman BJ, Mundis GM, Ames CP, Smith JS, Hart R, Burton D, Klineberg EO, International Spine Study G (2017) Perioperative neurologic complications in adult spinal deformity surgery: incidence and risk factors in 564 patients. Spine (Phila Pa 1976) 42(6):420–427
Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, Goodwin CR, Lafage V, Hart RA, Bess S, Kebaish K, Schwab F, Shaffrey CI, Ames CP, International Spine Study G (2015) A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform 3(6):575–594
Schwab FJ, Hawkinson N, Lafage V, Smith JS, Hart R, Mundis G, Burton DC, Line B, Akbarnia B, Boachie-Adjei O, Hostin R, Shaffrey CI, Arlet V, Wood K, Gupta M, Bess S, Mummaneni PV, International Spine Study G (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 21(12):2603–2610
Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH (2007) Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 32(20):2238–2244
Edwards CC 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG (2004) Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976) 29(18):1996–2005
Emami ADV, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976) 27(7):776–786
Acknowledgments
The author thank the invaluable support from Beijing Chaoyang Hospital affiliated to China Capital Medical University. The author thanks Dr. Yong Hai who supervised the study, provided technique support, and corrected some mistakes. The authors also thank Dr. Xiang-yao Sun and Xiang-long Meng for providing the analysis of the clinical data.
Funding
This study was supported partially by research fund provided by National Natural Science Foundation of China (NSFC) No. 81372008 and China Scholarship Council No. 201608110199.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was in accordance with the ethical standards of the institutional research committee, the 1964 Helsinki declaration, and its later amendments. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Zhang, Xn., Sun, Xy., Meng, Xl. et al. Risk factors for medical complications after long-level internal fixation in the treatment of adult degenerative scoliosis. International Orthopaedics (SICOT) 42, 2603–2612 (2018). https://doi.org/10.1007/s00264-018-3927-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3927-6