Abstract
Purpose
To assess the diagnostic image quality and material decomposition characteristics of portal venous phase abdominal CT scans performed on rapid kVp-switching DECT (rsDECT) in patients with large body habitus.
Methods
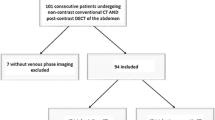
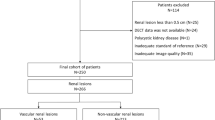
We retrospectively included consecutive patients with large body habitus (≥ 90 kg) undergoing portal venous phase abdominal CT scans on rsDECT scanners between Sep 2014 and March 2018. Qualitative and quantitative assessment of the DECT data sets [65 keV monoenergetic, material density iodine (MD-I) and material density water (MD-W) images] was performed for determination of image quality (IQ) and image noise. Correlation of qualitative assessment scores with weight, BMI and patients’ diameter were calculated using Pearson correlation test. Optimal thresholds were calculated using AUC and Youden index to define most appropriate size cut off, below which the IQ of material density images is largely acceptable.
Results
The 65 keV monoenergetic images were of diagnostic quality (diagnostic acceptability, DA ≥ 3) in 97.8% of patients (n = 91/93). However, there was significant IQ degradation of MD-I images in 20.4% (n = 19/93, DA < 3) of patients. Similarly, there was significant degradation (DA < 3) of MD-W images in 26.9% (25/92). Clinically significant artifacts (PA ≥ 3/4) were seen in 31% (n = 29/93) and 32.3% (30/93) of MD-I and MD-W images respectively. Optimal threshold for diagnostic acceptability of MD-I images were 110 kg for weight and 33.5 kg/m2 for BMI.
Conclusion
Rapid kVp-switching DECT provides diagnostically acceptable monoenergetic images for patients with large body habitus (≥ 90 kg). There is degradation of IQ in the material density specific images particularly in patients weighing > 110 kg and with BMI > 33.5 kg/m2, due to higher number of artifacts.




Similar content being viewed by others
Abbreviations
- MD-I:
-
Material density iodine
- MD-W:
-
Material density water
- IQ:
-
Image quality
- DA:
-
Diagnostic acceptability
- BMI:
-
Body mass index
- PA:
-
Presence of artifacts
- SAN:
-
Subjective analysis of image noise
- TD:
-
Transverse diameter
- DEFOV:
-
Dual energy field of view
- ASIR:
-
Adaptive statistical iterative reconstruction
References
Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011-2014. NCHS Data Brief. 2015 Nov;(219):1–8.
Obesity Update - OECD [Internet]. [cited 2018 Jul 16]. Available from: http://www.oecd.org/health/obesity-update.htm.
Defining Adult Overweight and Obesity | Overweight & Obesity | CDC [Internet]. [cited 2018 Jul 16]. Available from: https://www.cdc.gov/obesity/adult/defining.html
Rajapakse CS, Chang G. Impact of Body Habitus on Radiologic Interpretations. Acad Radiol. 2014 Jan;21(1):1–2.
Modica MJ, Kanal KM, Gunn ML. The Obese Emergency Patient: Imaging Challenges and Solutions. RadioGraphics. 2011 May 1;31(3):811–23.
Whiteman DC, Wilson LF. The fractions of cancer attributable to modifiable factors: A global review. Cancer Epidemiol. 2016;44:203–21.
Arnold M, Pandeya N, Byrnes G, Renehan PAG, Stevens GA, Ezzati PM, et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol. 2015 Jan;16(1):36–46.
Uppot RN. Impact of Obesity on Radiology. Radiol Clin. 2007 Mar 1;45(2):231–46.
The obesity epidemic: The role of radiology [Internet]. [cited 2018 Jul 16]. Available from: https://appliedradiology.com/articles/the-obesity-epidemic-the-role-of-radiology.
Hot Topic: Comparison of Single and Dual Source 64-Channel MDCT Scanners for Evaluation of Large Patients: A Phantom Study [Internet]. [cited 2018 Sep 25]. Available from: http://archive.rsna.org/2005/4425786.html
Pfeiffer D, Parakh A, Patino M, Kambadakone A, Rummeny EJ, Sahani DV. Iodine material density images in dual-energy CT: quantification of contrast uptake and washout in HCC. Abdom Radiol N Y. 2018 Dec;43(12):3317–23.
Parakh A, Patino M, Muenzel D, Kambadakone A, Sahani DV. Role of rapid kV-switching dual-energy CT in assessment of post-surgical local recurrence of pancreatic adenocarcinoma. Abdom Radiol N Y. 2018 Feb;43(2):497–504.
Muenzel D, Lo GC, Yu HS, Parakh A, Patino M, Kambadakone A, et al. Material density iodine images in dual-energy CT: Detection and characterization of hypervascular liver lesions compared to magnetic resonance imaging. Eur J Radiol. 2017 Oct;95:300–6.
Megibow AJ, Sahani D. Best Practice: Implementation and Use of Abdominal Dual-Energy CT in Routine Patient Care. Am J Roentgenol. 2012 Nov;199(5_supplement):S71–7.
Megibow AJ, Kambadakone A, Ananthakrishnan L. Dual-Energy Computed Tomography: Image Acquisition, Processing, and Workflow. Radiol Clin North Am. 2018 Jul;56(4):507–20.
Baliyan V, Shaqdan K, Hedgire S, Ghoshhajra B. Vascular computed tomography angiography technique and indications. Cardiovasc Diagn Ther. 2019 Aug;9(Suppl 1):S14–27.
Baliyan V, Kordbacheh H, Serrao J, Sahani DV, Kambadakone AR. Dual-Source Dual-Energy CT Portal Venous Phase Abdominal CT Scans in Large Body Habitus Patients: Preliminary Observations on Image Quality and Material Decomposition. J Comput Assist Tomogr. 2018 Dec;42(6):932–6.
Atwi NE, Smith DL, Flores CD, Dharaiya E, Danrad R, Kambadakone A, et al. Dual-energy CT in the obese: a preliminary retrospective review to evaluate quality and feasibility of the single-source dual-detector implementation. Abdom Radiol N Y. 2018 Sep 19.
Uppot RN, Sahani DV, Hahn PF, Kalra MK, Saini SS, Mueller PR. Effect of Obesity on Image Quality: Fifteen-year Longitudinal Study for Evaluation of Dictated Radiology Reports 1. Radiology. 2006;240(2):435–439.
Patino M, Fuentes JM, Singh S, Hahn PF, Sahani DV. Iterative Reconstruction Techniques in Abdominopelvic CT: Technical Concepts and Clinical Implementation. AJR Am J Roentgenol. 2015 Jul;205(1):W19-31.
Christe A, Heverhagen J, Ozdoba C, Weisstanner C, Ulzheimer S, Ebner L. CT dose and image quality in the last three scanner generations. World J Radiol. 2013 Nov 28;5(11):421–9.
Gervaise A, Naulet P, Beuret F, Henry C, Pernin M, Portron Y, et al. Low-dose CT with automatic tube current modulation, adaptive statistical iterative reconstruction, and low tube voltage for the diagnosis of renal colic: impact of body mass index. AJR Am J Roentgenol. 2014 Mar;202(3):553–60.
Goldman LW. Principles of CT: Radiation Dose and Image Quality. J Nucl Med Technol. 2007 Dec 1;35(4):213–25.
Kaza RK, Platt JF, Goodsitt MM, Al-Hawary MM, Maturen KE, Wasnik AP, et al. Emerging Techniques for Dose Optimization in Abdominal CT. Radiographics. 2014 Jan;34(1):4–17.
Silva AC, Lawder HJ, Hara A, Kujak J, Pavlicek W. Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol. 2010 Jan;194(1):191–9.
Desai GS, Uppot RN, Yu EW, Kambadakone AR, Sahani DV. Impact of iterative reconstruction on image quality and radiation dose in multidetector CT of large body size adults. Eur Radiol. 2012 Aug;22(8):1631–40.
Marin D, Nelson RC, Schindera ST, Richard S, Youngblood RS, Yoshizumi TT, et al. Low-tube-voltage, high-tube-current multidetector abdominal CT: improved image quality and decreased radiation dose with adaptive statistical iterative reconstruction algorithm--initial clinical experience. Radiology. 2010 Jan;254(1):145–53.
Desai GS, Fuentes Orrego JM, Kambadakone AR, Sahani DV. Performance of iterative reconstruction and automated tube voltage selection on the image quality and radiation dose in abdominal CT scans. J Comput Assist Tomogr. 2013 Dec;37(6):897–903.
Desai GS, Thabet A, Elias AYA, Sahani DV. Comparative assessment of three image reconstruction techniques for image quality and radiation dose in patients undergoing abdominopelvic multidetector CT examinations. Br J Radiol. 2013 Jan;86(1021):20120161.
Andrabi Y, Pianykh O, Agrawal M, Kambadakone A, Blake MA, Sahani DV. Radiation Dose Consideration in Kidney Stone CT Examinations: Integration of Iterative Reconstruction Algorithms With Routine Clinical Practice. AJR Am J Roentgenol. 2015 May;204(5):1055–63.
Shaqdan KW, Kambadakone AR, Hahn P, Sahani DV. Experience With Iterative Reconstruction Techniques for Abdominopelvic Computed Tomography in Morbidly and Super Obese Patients. J Comput Assist Tomogr. 2018 Feb;42(1):124–32.
Chen L-H, Jin C, Li J-Y, Wang G-L, Jia Y-J, Duan H-F, et al. Image quality comparison of two adaptive statistical iterative reconstruction (ASiR, ASiR-V) algorithms and filtered back projection in routine liver CT. Br J Radiol. 2018 Jul;91(1088):20170655.
Kordbacheh H, Baliyan V, Uppot RN, Eisner BH, Sahani DV, Kambadakone AR. Dual-Source Dual-Energy CT in Detection and Characterization of Urinary Stones in Patients With Large Body Habitus: Observations in a Large Cohort. Am J Roentgenol. 2019 Jan 23;1–6.
Tamm EP, Le O, Liu X, Layman RR, Cody DD, Bhosale PR. “How to” Incorporate Dual Energy Imaging Into a High Volume Abdominal Imaging Practice. Abdom Radiol N Y. 2017 Mar;42(3):688–701.
Van Der Kooy K, Leenen R, Seidell JC, Deurenberg P, Visser M. Abdominal diameters as indicators of visceral fat: comparison between magnetic resonance imaging and anthropometry. Br J Nutr. 1993 Jul;70(01):47.
Kordbacheh H, Baliyan V, Singh P, Eisner BH, Sahani DV, Kambadakone AR. Rapid kVp switching dual-energy CT in the assessment of urolithiasis in patients with large body habitus: preliminary observations on image quality and stone characterization. Abdom Radiol N Y. 2018 Nov 10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest. Avinash Kambadakone, MD, FRCR has following disclosures: Research Grant – Philips; Research Grant – GE Healthcare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Vinit Baliyan and Hamed Kordbacheh are co-first authors.
Rights and permissions
About this article
Cite this article
Baliyan, V., Kordbacheh, H., Pourvaziri, A. et al. Rapid kVp-switching DECT portal venous phase abdominal CT scans in patients with large body habitus: image quality considerations. Abdom Radiol 45, 2902–2909 (2020). https://doi.org/10.1007/s00261-020-02416-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02416-7