Abstract
Purpose
3′-Deoxy-3′-[18F]fluorothymidine positron emission tomography ([18F]FLT-PET) has been developed for imaging cell proliferation and findings correlate strongly with the Ki-67 labelling index in breast cancer. The aims of this pilot study were to define objective criteria for [18F]FLT response and to examine whether [18F]FLT-PET can be used to quantify early response of breast cancer to chemotherapy.
Methods
Seventeen discrete lesions in 13 patients with stage II–IV breast cancer were scanned prior to and at 1 week after treatment with combination 5-fluorouracil, epirubicin and cyclophosphamide (FEC) chemotherapy. The uptake at 90 min (SUV90) and irreversible trapping (K i) of [18F]FLT were calculated for each tumour. The reproducibility of [18F]FLT-PET was determined in nine discrete lesions from eight patients who were scanned twice before chemotherapy. Clinical response was assessed at 60 days after commencing FEC.
Results
All tumours showed [18F]FLT uptake and this was reproducible in serial measurements (SD of mean % difference = 10.5% and 15.1%, for SUV90 and K i, respectively; test–retest correlation coefficient ≥0.97). Six patients had a significant clinical response (complete or partial) at day 60; these patients also had a significant reduction in [18F]FLT uptake at 1 week. Decreases in K i and SUV90 at 1 week discriminated between clinical response and stable disease (p = 0.022 for both parameters). In three patients with multiple lesions there was a mixed [18F]FLT response in primary tumours and metastases. [18F]FLT response generally preceded tumour size changes.
Conclusion
[18F]FLT-PET can detect changes in breast cancer proliferation at 1 week after FEC chemotherapy.
Similar content being viewed by others
Introduction
Breast cancer is a leading cause of cancer death in women in the industrialised world; one in eight women will develop breast cancer at some stage during their lifetime. Approximately 30% of patients who present with locoregional disease will develop metastases [1], and despite recent advances in treatment, the vast majority of these patients will be incurable.
Response to chemotherapy of large primary tumours and locally advanced and metastatic disease is routinely measured using the RECIST criteria [2], which rely on changes in the measured sum of the longest diameters of the target lesion(s). Physical changes in tumour dimensions after chemotherapy and hormonal therapy may, however, take a long time to develop, and may not provide any indication of the viability of residual tumour mass. Indeed, the RECIST criteria may be altogether inappropriate for the assessment of molecular therapeutics that do not shrink tumours [3].
Measurement of cell proliferation could provide an alternative strategy for detecting chemosensitivity or chemoresistance of breast tumours, an important consideration in understanding an individual patient’s treatment response benefit and hence in minimising patient exposure to ineffective and potentially toxic treatment regimens. In this regard, proliferation measurements will be most useful when determined early in the course of treatment. Histological Ki-67 immunostaining and analysis of cell cycle genes have shown changes in breast tumour proliferation status as early as 24 h and certainly at 1–4 weeks after chemotherapy or hormone therapy; in some cases the early changes in proliferation were predictive of pathological response [4–8].
Molecular imaging methods such as [18F]fluorodeoxyglucose positron emission tomography ([18F]FDG-PET) have been explored as surrogates to the anatomical and histological or molecular approaches mentioned above owing to a combination of factors including their non-invasive nature, their ability to detect changes in tumour biochemistry in all tumour regions and their good reproducibility [9, 10]. Decreases in [18F]FDG uptake as early as 1 week after starting treatment have previously been reported in breast tumours [9]. [18F]FDG uptake may, however, increase within the early period after treatment through mechanisms involving an enhanced inflammatory response, making it unpredictable as a response marker [11, 12]. Proliferation markers like the thymidine analogue, 3′-deoxy-3′-[18F]fluorothymidine ([18F]FLT), are not susceptible to such inflammatory changes [13] and can potentially be used to measure early changes in response. We have recently shown that [18F]FLT can be used to measure proliferation in tumours of breast cancer patients [14]. The current study examines the role of [18F]FLT for determining response to therapy in breast cancer; in this specific instance a standard chemotherapy regimen [5-fluorouracil, epirubicin and cyclophosphamide (FEC)] was used. To ascertain whether the reductions in [18F]FLT uptake post treatment are significant, knowledge of the intrinsic variability of [18F]FLT-PET is required. No such data have been reported for breast or any other cancer. In this study we have for the first time determined the reproducibility of serial [18F]FLT-PET measurements in breast tumours and used these to provide the objective criteria for early response assessment.
A previous [18F]FLT-PET study evaluated response of breast tumours to a variety of treatments (chemotherapy and endocrine therapy) at 5.5 weeks [15]. The timescale for post-treatment scans in that study was similar to that for RECIST [2]. We rationalised that, like the early [18F]FDG studies [9], oncologists may benefit more from an earlier indication of response. Thus, in our current study, we investigated whether [18F]FLT-PET could be used to measure response as early as 1 week after initiation of FEC chemotherapy and compared the PET results with clinical response measured at 60 days.
Materials and methods
Patients
We studied 15 patients attending the Hammersmith & Charing Cross Hospitals, London, UK. Patients aged between 18 and 80 who had histologically proven American Joint Committee on Cancer (AJCC) stage II–IV breast cancer [16] and were to be treated with FEC chemotherapy were eligible, with sites of metastases outside the liver or bone marrow (Table 1). All patients had at least one lesion with a minimum diameter of 2.5 cm in diameter. Patients were not receiving active treatment at the time of the study; there was a treatment-free interval of not less than 3 weeks for effective cytotoxic chemotherapy or hormonal therapy, and 4 weeks for radiotherapy. All patients were expected to have a life expectancy of at least 3 months and an Eastern Cooperative Oncology Group performance status of 0–2 inclusive. Satisfactory haematological indices were defined as haemoglobin ≥10 g·dl−1, granulocyte count ≥1.5 × 109 l−1, platelet count ≥100 × 109 l−1, adequate creatinine clearance (calculated ≥50 ml·min−1) and adequate hepatic function (bilirubin ≤25 IU/l, serum transaminases ≤70 IU/l). Patients who were pregnant, lactating or not practising adequate contraception were excluded from the study. Patients gave written informed consent to take part in the study, which had approval form the Hammersmith Hospital Research Ethics Committee and the Administration of Radioactive Substances Advisory Committee (ARSAC), UK. The studies were conducted according to the Declaration of Helsinki.
Study design
The aims of the study were to (a) determine the reproducibility of serial [18F]FLT-PET scans to define objective [18F]FLT-PET response and (b) determine [18F]FLT-PET response at 1 week in patients treated with chemotherapy. To achieve these aims, three [18F]FLT-PET scans were scheduled for each patient. Two reproducibility scans were performed within 2–8 days of each other prior to commencement of treatment. Patients were then treated with standard combination intravenous 5-fluorouracil (600 mg/m2), epirubicin (60 mg/m2) and cyclophosphamide (600 mg/m2) (FEC) chemotherapy. The last PET scan was performed at approximately 1 week after starting chemotherapy. Patients continued to receive FEC chemotherapy every 21 days up to a maximum of eight cycles until surgery or disease progression.
PET imaging and blood sampling
All PET scans were performed as outpatient procedures. An arterial cannula was inserted into the radial artery under local anaesthesia for blood sampling before scanning; a venous cannula was inserted for injection of radioactivity. [18F]FLT was synthesised by Hammersmith Imanet by radiofluorination of the 2,3′-anhydro-5′-O-(4,4′-dimethoxytrityl)-thymidine precursor using a method previously described by Cleij et al. [17]. All patients received a single bolus intravenous injection of [18F]FLT (153–381 MBq, specific activity 15–227 GBq·μmol−1) over 30 s, and PET scanning was performed for 95 min. Patients were scanned on an ECAT962/HR+ PET scanner (CTI/Siemens, Knoxville, TN), which allows simultaneous data acquisition to form 63 transaxial planes (axial field of view 15.5 cm; transaxial 58 cm). Data were binned into 31 discrete time intervals of varying duration (30 s × 10, 60 s × 5, 120 s × 5, 180 s × 5, 600 s × 6). From the summed PET image data, regions of interest on tumour tissues were defined manually using the Analyze image analysis software (Biomedical Imaging Resource, Mayo Foundation Rochester, MN, USA) and applied to the dynamic data to obtain a time versus radioactivity curve (TAC) by the same observer. All planes with identifiable tumour uptake were measured. To derive an arterial input function, arterial blood sampling was performed continuously for the first 10 min of PET scanning; discrete arterial samples (10 ml) were taken at baseline, 2.5, 5, 10, 20, 30, 45, 60, 75 and 90 min. Total blood radioactivity was monitored by gamma counting and plasma [18F]FLT parent fraction (and metabolite, [18F]FLT-glucuronide) was determined by reverse-phase high-performance liquid chromatography with radiochemical detection as described previously [14]. These data were used to determine the parent plasma input function and total plasma input function.
Determination of kinetic parameters and statistical analyses
One of the objectives of this study was to determine the variability of different [18F]FLT retention parameters: a semi-quantitative standardised uptake value (SUV) and fully quantitative net irreversible plasma to tumour transfer constant (K i). SUV at 90 min, SUV90 (m2·ml−1), was calculated from the TAC as previously described [14]. K i (ml of plasma·s−1·ml tissue−1) was determined by a modified Patlak analysis, as previously described [14].
Analysis of reproducibility of SUV90 and K i was performed on a lesion-by-lesion basis. For reproducibility measurements, individual SUV90 and K i values for the two pre-treatment scans were plotted against each other; high reproducibility was represented by all data distributed along a line of unity. A Pearson’s correlation coefficient and Wilcoxon signed rank test were used to assess reproducibility. We also assessed normality of the data as a probability plot of the ordered relative differences versus the normal probability (cumulative frequency of ranks) for each lesion. Relative differences in parameter estimates were defined as 2×(Scan A−Scan B)/(Scan A+Scan B). A box-and-whiskers plot of relative difference in SUV90 and K i was performed to illustrate parameter variability. To compare the reproducibility of the two parameters, SUV90 and K i, an intraclass correlation coefficient (IC) that describes the correlation between the two measurements of a parameter was calculated; if the two measurements are identical, the IC will be 1. Random or systematic differences between the two measurements reduce the value of the IC. A two-way random mixed model with absolute agreement was used. The difference in the variance of the relative difference for the different parameters was tested using the F test, which compares the standard deviations (SDs) of two normally distributed data sets.
The 95% normal ranges for spontaneous fluctuations in SUV90 and K i was calculated as 1.96×SD of the relative difference in the two pre-treatment scans. [18F]FLT response was the relative difference between post-treatment and mean pre-treatment measurement parameters, i.e. 2×(Scanpre−Scanpost)/(Scanpre), where the pre-treatment scan is the mean of the two pre-treatment scans in the case of patients who completed the reproducibility phase of the study. The Mann-Whitney test was used to assess the significance of the change in [18F]FLT uptake between (a) clinical responders (complete or partial, CR/PR) and (b) stable disease. A p value of ≤0.05 was considered significant. Statistical analyses were performed using SPSS for Windows version 12 (SPSS, Chicago, IL, USA) and GraphPad Prism version 3.0 (Graph Pad Software, San Diego, CA, USA).
Clinical response
Tumour response was defined using the RECIST criteria [2]. Tumours were measured using electronic calipers (AR/2001, Camlab Laboratory products, Cambridge, UK) on each of the PET scanning visits and at day 60 post treatment by the same investigator. Computed tomography was used in the case of a lung metastasis in patient 2.
Results
Fifteen patients with 19 discrete lesions due to breast cancer (all histological types; see Table 1 for demographics) were entered into the study. Of these, 13 had at least one pre-treatment and a post-treatment scan (one patient withdrew from the study owing to a viral illness and the other patient could not be scanned at 1 week). All of the patients tolerated the PET scanning protocol, and none suffered complications due to the study. Patients were aged between 37 and 80 years. With the exception of four patients (two with metastatic disease and two with locally advanced disease) who had received prior treatment for breast cancer, all patients were newly diagnosed.
Reproducibility of [18F]FLT-PET parameters
[18F]FLT was retained in all the breast tumours studied. As previously reported, high radiotracer localisation was also seen in the liver (due to glucuronidation) and bone (due to marrow poiesis) [14, 18]. Nine tumours from eight patients could be evaluated for reproducibility of repeated measures of [18F]FLT retention; other tumours could not be evaluated owing to [18F]FLT production failures and/or inability to schedule a second PET scan prior to patients commencing therapy. The time between baseline scan and the reproducibility scan ranged from 2 to 10 (median 4.5) days. Figure 1a and b show plots of K i and SUV90 at the two pre-treatment measurement periods. For neither imaging parameter was there a significant difference between the two scans (p = 0.95 for SUV90 and 1.05 for K i). Regression analysis of the line of unity indicated good test–retest correlation (r = 0.99 for SUV90 and 0.97 for K i). The variability of the relative difference is shown in Fig. 1c. The standard deviations of the mean relative difference were 10.5% and 15.1% for SUV90 and K i, respectively. The ICs (single measures) for SUV90 and K i were 0.99 and 0.97, respectively. The coefficient of repeatability was 1.999 for SUV90 and 1.497 for K i. F test values were 0.97 for SUV90 and 0.99 for K i. These results indicate that both parameters (SUV90 and K i) can be used repeatedly in serial scans. The relative differences in imaging parameters were found to be normally distributed [goodness of fit r 2 = 0.97 and 0.96 for SUV90 and K i; p (runs test) >0.5 for both parameters, i.e. not significantly non-linear]. The 95% normal values for spontaneous fluctuations were determined from the SD of the relative difference in K i and SUV90 as ±0.297 × 10−4 ml plasma·s−1·ml tissue−1 and ±0.206 × 10−5 m2·ml−1, respectively.
Reproducibility of [18F]FLT-PET scanning parameters. Correlation between baseline (scan 1) and repeat scan (scan 2) for: a K i and b SUV90. c A box and whiskers plot of the variability of K i and SUV90. The error bars are 95% confidence intervals; the horizontal line within each box is the median variability
Clinical and [18F]FLT-PET response
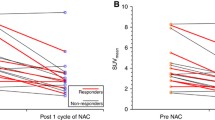
Thirteen patients completed both pre-treatment and post-treatment scans at the required study time. Clinical response (CR/PR) was evident in six patients at 60 days; of the remaining patients, six had stable disease and one died from cerebral metastases. Therefore, no patient could be classified as having had progressive disease within the imaging region. The interval between commencement of chemotherapy and the post-treatment [18F]FLT-PET scanning ranged from 6 to 12 (median 8) days. Figure 2a and b show typical transverse PET images through the chest of patient 1 before and after receiving FEC chemotherapy; a reduction in [18F]FLT uptake was seen at 1 week post treatment. This patient showed the most significant [18F]FLT-PET response, with an 83% decrease in [18F]FLT uptake. Figure 2c and d are images of patient 8, who did not show a reduction in [18F]FLT uptake. The average SUV90 and K i from multiple slices of entire lesions were compared. Figure 3 shows the [18F]FLT-PET response pattern for all lesions. Objective [18F]FLT response was defined as relative differences in imaging parameters that were below the normal ranges of spontaneous fluctuation; values higher than the range constituted significantly increased proliferation. The normal ranges are the two solid lines on either side of the mean (bold solid line) in Fig. 3. [18F]FLT-PET response (<95% range) was seen in 12 of 17 (SUV90) and 11 of 17 ( K i) lesions. In responding lesions the average decrease in FLT-PET was 41.3% for SUV90 and 52.9% for K i; in non-responding lesions the average increase in FLT-PET was 3.1% for SUV90 and 1.9% for K i (Fig. 3). As there were no changes in tumour size at 1 week (Table 2), with the exception of the axillary metastasis in patient 6, we can state that the [18F]FLT-PET responses preceded tumour size changes.
[18F]FLT-PET images in responding and non-responding patients. a Pre-treatment and b post-treatment images of a patient with grade II lobular carcinoma that responded to treatment. c Pre-treatment and d post-treatment images of a patient with grade II invasive ductal carcinoma that did not respond to treatment
Relative differences in [18F]FLT-PET parameters in individual lesions. The changes in a K i ( × 10−4 ml plasma·s−1·ml tissue−1) and b SUV (SUV90 × 10−5 m2·ml−1) were plotted. [18F]FLT-PET response was defined using the coefficient of repeatability. The shaded areas on either side of the median (bold line) represent normal variability
All six patients who had a clinical response also had a significant reduction in [18F]FLT uptake as measured by K i and SUV. Figure 4 shows the relationship between [18F]FLT response and clinical response of individual lesions. Pre-treatment tumour size and tumour sizes at days 8 and 60 post chemotherapy are recorded in Table 2. Only one of the patients (patient 2) in this study developed progressive disease after the first cycle of treatment in the form of previously undiagnosed cerebral metastases and died as a result of this before day 60; the metastases were outside the field of view of the PET scanner used in this study. Patient 12 withdrew from study owing to a viral illness, and patient 15 developed a breast abscess after the first cycle of chemotherapy and proceeded to mastectomy. Although the abscess was in the breast region, the patient did not develop any clinical evidence of an abscess until the next cycle of treatment; there had been no ultrasonic findings of an abscess on pre-treatment scanning. These patients could not be assessed for clinical response to FEC at day 60. Patient 3 had a significant increase in K i and SUV90 by 92.3% and 69.2%, respectively; this patient failed to achieve a partial response, and had disease progression within 18 months following completion of chemotherapy.
Changes in [18F]FLT uptake were not always similar for different lesions in patients with more than one lesion, i.e. there was intra-patient variability in [18F]FLT response. This was evident in patients 5, 6 and 10 for both K i and SUV90. For instance, patient no. 5 had a primary lobular carcinoma with axillary nodal and internal mammary metastases (the internal mammary metastasis had not been detected on prior screening investigations, including computed tomography). Clinically the patient was classified as a non-responder owing to lack of response in the primary tumour (although the axillary node showed a reduction in size) after two cycles of FEC, and her treatment was changed to combination docetaxel–trastuzumab. With regard to [18F]FLT response, the primary tumour did not show a significant reduction in K i or SUV90, whereas there was a significant reduction in SUV90 and K i in the internal mammary node and the axillary nodal metastasis. Similarly, patient 6 had a reduction in both SUV90 and K i in the axilla but not in the breast; this patient had a clinical response in both areas. The patient has subsequently relapsed in the breast despite completing six cycles of chemotherapy plus surgery and radiotherapy. It was interesting to note at the time of surgery that this patient had a pathological complete response in the axilla.
To evaluate the early predictive value of [18F]FLT-PET in breast cancer patients, i.e. the ability of PET at 1 week post treatment to predict response at 60 days, we classified the lesions in this pilot study into CR/PR (n = 7 lesions) and those with stable disease at day 60 (n = 6 lesions), and compared the results with early [18F]FLT response. Figure 4 shows that there was a significant difference between the two groups regarding changes in [18F]FLT parameters (Mann-Whitney p = 0.022 for both K i and SUV90).
Discussion
We have shown in this pilot study in patients with breast cancer that (a) early changes in response at 1 week are detectable by [18F]FLT-PET and that this precedes physical changes in tumour diameter and (b) serial studies of [18F]FLT-PET scanning can be performed with high reproducibility. [18F]FLT is a radiolabelled thymidine analogue that is being investigated for measurement of cellular proliferation. We have recently reported that in patients with breast cancer, tumour [18F]FLT uptake significantly correlates with cellular proliferation measured as the Ki-67 labelling index, with correlation coefficients of 0.92 for K i and 0.79 for SUV90 [14]. In this manuscript we sought to investigate whether [18F]FLT-PET could be used clinically to image early changes in response to therapy.
Knowledge of the precision of repeated measurements of imaging parameters is a prerequisite for serial measurements and hence reliable detection of response. Neither SUV90 nor K i showed a significant increase or decrease between the two pre-treatment scans or deviation from normality. Our study shows that serial [18F]FLT-PET studies can be done with high reproducibility; the 95% normal range of spontaneous fluctuations was 10.5% and 15.1% for SUV90 and K i. Unlike the higher accuracy of using K i for predicting proliferation [14], however, there was no clear advantage to using modelled data where precision of measurements was concerned. However, K i is the more accurate parameter when correlated with Ki-67 labelling index [14]. Factors that can affect the SUV90 parameter include changes in radiotracer delivery and dephosphorylation within the tumour, as well as changes in systemic clearance after treatment. Hence, the more clinically applicable method, SUV, is robust but knowledge of the aforementioned factors needs to be obtained to justify its use.
In this study, [18F]FLT objective response was defined as a change in SUV90 or K i that was outside the 95% limits. In general a lesion parameter change of ≥18% for SUV and 31% for K i will be outside this range and can be classified as [18F]FLT response. This is the first report of [18F]FLT reproducibility in any cancer type. Weber et al. and Minn et al. have reported a similar level of reproducibility for [18F]FDG-PET in diverse tumour types [10, 19]. 2-[11C]thymidine-PET has also been shown to be reproducible, with an IC ≥0.95 for semi-quantitative and modelled data [20].
Objective changes in [18F]FLT-PET were seen at 1 week after FEC chemotherapy. Given that [18F]FLT uptake highly correlated with proliferation in breast cancer in our previous study [14], the present findings indicate that [18F]FLT-PET can be used to measure changes in proliferation as early as 1 week post treatment. Since tumours can acquire drug resistance after 1 week of treatment, this time point is not necessarily optimal for imaging but allows for early monitoring of chemosensitivity. [18F]FLT-PET response was seen in a high proportion of tumours at this early time point (12 of 17 or 11 of 17 when assessed by SUV90 or K i) and importantly preceded tumour size changes. In our study, the treatment for patients with primary and patients with metastatic breast cancer was the same, and no patient in either group had received this type of combination chemotherapy within the 2 months preceding the imaging study. Furthermore, each patient had a scan prior to treatment and one during treatment, thus removing any bias due to differences in baseline proliferation. Although this was a pilot study, we sought to compare the [18F]FLT-PET lesion response to the patient’s clinical response at 60 days. In general the patients who showed CR/PR had a change in SUV90 and K i of −63.4% to −15.6% and −83.0% to −20.4%, respectively. The absence of patients with clear tumour progression is a limitation of this study as it did not permit us to make definitive statements about [18F]FLT-PET profiles in progressive disease.
Our ability to distinguish the patients with stable disease and those with CR/PR at 1 week post treatment with [18F]FLT-PET is of relevance in a clinical setting. Changes in proliferation-related processes have been detected by other technologies. For instance, reductions in Ki-67 labelling index and [18F]FDG-PET have been reported within similar time frames [4–8, 21]. [18F]FLT-PET should be superior to [18F]FDG-PET within this time frame owing to its higher specificity for proliferation and its insensitivity to treatment-induced inflammatory changes [13, 22]. Pio et al. have recently reported the advantage of [18F]FLT-PET over [18F]FDG-PET using the SUV parameter for measurement of treatment response in breast cancer at ∼5 weeks post treatment [15]. Although both our study and that of Pio et al. involved relatively small numbers of patients, they demonstrate the potential of [18F]FLT-PET for assessment of proliferation and support its use in larger clinical trials to determine the impact of the technology in assessing early response to therapy.
In conclusion, we have demonstrated in this pilot study that:
-
Serial [18F]FLT-PET studies can be done with high reproducibility in patients with breast cancer.
-
[18F]FLT-PET can detect changes in proliferation at 1 week post treatment after FEC chemotherapy.
References
Surveillance E, End Results (SEER) Program (http://www.seer.cancer.gov). SEER*Stat Database: Incidence-SEER 17 Regs Public-Use, Nov 2005 Sub (1973–2003 varying), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2006, based on the November 2005 submission.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 2000;92:205–16.
Korn EL, Arbuck SG, Pluda JM, Simon R, Kaplan RS, Christian MC. Clinical trial designs for cytostatic agents: are new approaches needed? J Clin Oncol 2001;19:265–72.
Dowsett M, Archer C, Assersohn L, Gregory RK, Ellis PA, Salter J, et al. Clinical studies of apoptosis and proliferation in breast cancer. Endocr Relat Cancer 1999;6:25–8.
Ellis MJ, Coop A, Singh B, Tao Y, Llombart-Cussac A, Janicke F, et al. Letrozole inhibits tumor proliferation more effectively than tamoxifen independent of HER1/2 expression status. Cancer Res 2003;63:6523–31.
Ellis MJ, Rosen E, Dressman H, Marks J. Neoadjuvant comparisons of aromatase inhibitors and tamoxifen: pretreatment determinants of response and on-treatment effect. J Steroid Biochem Mol Biol 2003;86:301–7.
van Diest PJ, van der Wall E, Baak JP. Prognostic value of proliferation in invasive breast cancer: a review. J Clin Pathol 2004;57:675–81.
Vincent-Salomon A, Rousseau A, Jouve M, Beuzeboc P, Sigal-Zafrani B, Freneaux P, et al. Proliferation markers predictive of the pathological response and disease outcome of patients with breast carcinomas treated by anthracycline-based preoperative chemotherapy. Eur J Cancer 2004;40:1502–8.
Wahl RL, Zasadny K, Helvie M, Hutchins GD, Weber B, Cody R. Metabolic monitoring of breast cancer chemohormonotherapy using positron emission tomography: initial evaluation. J Clin Oncol 1993;11:2101–11.
Weber WA, Ziegler SI, Thodtmann R, Hanauske AR, Schwaiger M. Reproducibility of metabolic measurements in malignant tumors using FDG PET. J Nucl Med 1999;40:1771–7.
Dehdashti F, Flanagan FL, Mortimer JE, Katzenellenbogen JA, Welch MJ, Siegel BA. Positron emission tomographic assessment of “metabolic flare” to predict response of metastatic breast cancer to antiestrogen therapy. Eur J Nucl Med 1999;26:51–6.
Spaepen K, Stroobants S, Dupont P, Bormans G, Balzarini J, Verhoef G, et al. [18F]FDG PET monitoring of tumour response to chemotherapy: does [18F]FDG uptake correlate with the viable tumour cell fraction? Eur J Nucl Med Mol Imaging 2003;30:682–8.
van Waarde A, Cobben DC, Suurmeijer AJ, Maas B, Vaalburg W, de Vries EF, et al. Selectivity of 18F-FLT and 18F-FDG for differentiating tumor from inflammation in a rodent model. J Nucl Med 2004;45:695–700.
Kenny LM, Vigushin DM, Al-Nahhas A, Osman S, Luthra SK, Shousha S, et al. Quantification of cellular proliferation in tumor and normal tissues of patients with breast cancer by [18F]fluorothymidine-positron emission tomography imaging: evaluation of analytical methods. Cancer Res 2005;65:10104–12.
Pio BS, Park CK, Pietras R, Hsueh WA, Satyamurthy N, Pegram MD, et al. Usefulness of 3′-[F-18]fluoro-3′-deoxythymidine with positron emission tomography in predicting breast cancer response to therapy. Mol Imaging Biol 2006;8:36–42.
Singletary SE, Allred C, Ashley P, Bassett LW, Berry D, Bland KI, et al. Revision of the American Joint Committee on Cancer staging system for breast cancer. J Clin Oncol 2002;20:3628–36.
Cleij MC, Steel CJ, Brady F, Ell PJ, Pike VW, Luthra SK. An improved synthesis of 3′-deoxy-3′-[18F]fluorothymidine ([18F]FLT) and the fate of the precursor 2,3′-anhydro-5′-O-(4,4′-dimethoxytrityl)-thymidine. J Labelled Compounds Radiopharm 2001;44 Suppl 1:871–3.
Shields AF, Grierson JR, Muzik O, Stayanoff JC, Lawhorn-Crews JM, Obradovich JE, et al. Kinetics of 3′-deoxy-3′-[F-18]fluorothymidine uptake and retention in dogs. Mol Imaging Biol 2002;4:83–9.
Minn H, Zasadny KR, Quint LE, Wahl RL. Lung cancer: reproducibility of quantitative measurements for evaluating 2-[F-18]-fluoro-2-deoxy-D-glucose uptake at PET. Radiology 1995;196:167–73.
Wells P, Gunn RN, Steel C, Ranicar AS, Brady F, Osman S, et al. 2-[11C]thymidine positron emission tomography reproducibility in humans. Clin Cancer Res 2005;11:4341–7.
Archer CD, Parton M, Smith IE, Ellis PA, Salter J, Ashley S, et al. Early changes in apoptosis and proliferation following primary chemotherapy for breast cancer. Br J Cancer 2003;89:1035–41.
Buck AK, Halter G, Schirrmeister H, Kotzerke J, Wurziger I, Glatting G, et al. Imaging proliferation in lung tumors with PET: 18F-FLT versus 18F-FDG. J Nucl Med 2003;44:1426–31.
Acknowledgements
This study was supported by the UK Medical Research Council (MRC), London, and we are grateful for this support. R.C.C.’s and E.O.A.’s research is also funded by CRUK.
We wish to express our gratitude to the patients, radiographers and staff at Hammersmith Imanet Ltd, without whom this study would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kenny, L., Coombes, R.C., Vigushin, D.M. et al. Imaging early changes in proliferation at 1 week post chemotherapy: a pilot study in breast cancer patients with 3′-deoxy-3′-[18F]fluorothymidine positron emission tomography. Eur J Nucl Med Mol Imaging 34, 1339–1347 (2007). https://doi.org/10.1007/s00259-007-0379-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0379-4