Abstract
Objective
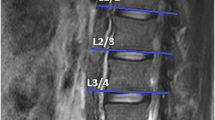
To reveal the best-suited method for fat quantification of lumbar multifidus to demonstrate its relationship to herniated nucleus pulposus (HNP) using T2-weighted Dixon.
Materials and methods
One hundred eight patients who underwent MRI for low back pain were enrolled. Two readers independently analyzed the fat fraction (Ff) using axial two-dimensional (D), coronal 2-D, and coronal 3-D measurement. Pearson’s correlation coefficient was calculated between age, body mass index (BMI), and the Ff, and age, sex, BMI, and Ff were compared between ‘HNP group’ and ‘no HNP group’. Multivariate logistic regression analysis was performed to identify factors associated with HNP.
Results
Coronal 2-D Ff showed the highest correlation with age (r = 0.536, P < 0.001). Coronal 2-D Ff, and coronal 3-D Ff were significantly higher in those with HNP (coronal 2-D: 18.9 ± 2.9, coronal 3-D: 19.7 ± 2.6, respectively) than those without HNP (coronal 2-D: 17.2 ± 3.2, coronal 3-D: 17.4 ± 3.2, respectively). Ff of all three measurements were significantly higher in those with HNP ≥ 3 levels (axial 2-D: 20.7 ± 3.0, coronal 2-D: 21.1 ± 2.7, coronal 3-D: 21.6 ± 2.5, respectively) than those with HNP <3 levels (axial 2-D: 17.5 ± 4.3, coronal 2-D: 18.5 ± 2.7, coronal 3-D: 19.3 ± 2.5). The BMI was an independent predisposing factor to HNP (P = 0.011). Age and coronal 2-D Ff were significant predictors for multilevel HNP (P = 0.028 and 0.040, respectively).
Conclusions
The Ff of the multifidus muscle on T2-weighted Dixon was associated with age, sex, and HNP. The coronal 2-D measurement was the best suited for fat quantification in multifidus muscle among three measurement methods.






Similar content being viewed by others
References
Crawford RJ, Filli L, Elliott JM, et al. Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol. 2016;37:742–8.
Teichtahl AJ, Urquhart DM, Wang Y, et al. Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J. 2015;15:1593–601.
Fortin M, Lazary A, Varga PP, McCall I, Battie MC. Paraspinal muscle asymmetry and fat infiltration in patients with symptomatic disc herniation. Eur Spine J. 2016;25:1452–9.
Ekin EE, Kurtul Yildiz H, Mutlu H. Age and sex-based distribution of lumbar multifidus muscle atrophy and coexistence of disc hernia: an MRI study of 2028 patients. Diagn Interv Radiol. 2016;22:273–6.
Altinkaya N, Cekinmez M. Lumbar multifidus muscle changes in unilateral lumbar disc herniation using magnetic resonance imaging. Skelet Radiol. 2016;45:73–7.
Takayama K, Kita T, Nakamura H, et al. New predictive index for lumbar Paraspinal muscle degeneration associated with aging. Spine (Phila Pa 1976). 2016;41:E84–90.
Sasaki T, Yoshimura N, Hashizume H, et al. MRI-defined paraspinal muscle morphology in Japanese population: the Wakayama spine study. PLoS One. 2017;12:e0187765.
Urrutia J, Besa P, Lobos D, et al. Lumbar paraspinal muscle fat infiltration is independently associated with sex, age, and inter-vertebral disc degeneration in symptomatic patients. Skelet Radiol. 2018;47:955–61.
Paalanne N, Niinimaki J, Karppinen J, et al. Assessment of association between low back pain and paraspinal muscle atrophy using opposed-phase magnetic resonance imaging: a population-based study among young adults. Spine (Phila Pa 1976). 2011;36:1961–8.
Elliott JM, Courtney DM, Rademaker A, Pinto D, Sterling MM, Parrish TB. The rapid and progressive degeneration of the cervical multifidus in whiplash: an MRI study of fatty infiltration. Spine (Phila Pa 1976). 2015;40:E694–700.
Abbott R, Peolsson A, West J, et al. The qualitative grading of muscle fat infiltration in whiplash using fat and water magnetic resonance imaging. Spine J. 2018;18:717–25.
Prasarn ML, Kostantinos V, Coyne E, Wright J, Rechtine GR. Does lumbar paraspinal muscle fatty degeneration correlate with aerobic index and Oswestry disability index? Surg Neurol Int. 2015;6:S240–3.
Suh DW, Kim Y, Lee M, Lee S, Park SJ, Yoon B. Reliability of histographic analysis for paraspinal muscle degeneration in patients with unilateral back pain using magnetic resonance imaging. J Back Musculoskelet Rehabil. 2017;30:403–12.
Takashima H, Takebayashi T, Ogon I, et al. Analysis of intra and extramyocellular lipids in the multifidus muscle in patients with chronic low back pain using MR spectroscopy. Br J Radiol. 2018;91:20170536.
Yanik B, Keyik B, Conkbayir I. Fatty degeneration of multifidus muscle in patients with chronic low back pain and in asymptomatic volunteers: quantification with chemical shift magnetic resonance imaging. Skelet Radiol. 2013;42:771–8.
Takashima H, Takebayashi T, Ogon I, et al. Evaluation of intramyocellular and extramyocellular lipids in the paraspinal muscle in patients with chronic low back pain using MR spectroscopy: preliminary results. Br J Radiol. 2016;89:20160136.
Fischer MA, Nanz D, Shimakawa A, et al. Quantification of muscle fat in patients with low back pain: comparison of multi-echo MR imaging with single-voxel MR spectroscopy. Radiology. 2013;266:555–63.
Wan Q, Lin C, Li X, Zeng W, Ma C. MRI assessment of paraspinal muscles in patients with acute and chronic unilateral low back pain. Br J Radiol. 2015;88:20140546.
Battie MC, Niemelainen R, Gibbons LE, Dhillon S. Is level- and side-specific multifidus asymmetry a marker for lumbar disc pathology? Spine J. 2012;12:932–9.
Goubert D, De Pauw R, Meeus M, et al. Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J. 2017;17:1285–96.
Urrutia J, Besa P, Lobos D, Andia M, Arrieta C, Uribe S. Is a single-level measurement of paraspinal muscle fat infiltration and cross-sectional area representative of the entire lumbar spine? Skelet Radiol. 2018;47:939–45.
Matsumura N, Oguro S, Okuda S, et al. Quantitative assessment of fatty infiltration and muscle volume of the rotator cuff muscles using 3-dimensional 2-point Dixon magnetic resonance imaging. J Shoulder Elb Surg. 2017;26:e309–e18.
Vidt ME, Santago AC 2nd, Tuohy CJ, et al. Assessments of fatty infiltration and muscle atrophy from a single magnetic resonance image slice are not predictive of 3-dimensional measurements. Arthroscopy. 2016;32:128–39.
Kushchayev SV, Glushko T, Jarraya M, et al. ABCs of the degenerative spine. Insights Imaging. 2018;9:253–74.
Ma J, Son JB, Bankson JA, Stafford RJ, Choi H, Ragan D. A fast spin echo two-point Dixon technique and its combination with sensitivity encoding for efficient T2-weighted imaging. Magn Reson Imaging. 2005;23:977–82.
Lee S, Choi DS, Shin HS, Baek HJ, Choi HC, Park SE. FSE T2-weighted two-point Dixon technique for fat suppression in the lumbar spine: comparison with SPAIR technique. Diagn Interv Radiol. 2018;24:175–80.
Maeder Y, Dunet V, Richard R, Becce F, Omoumi P. Bone marrow metastases: T2-weighted Dixon spin-echo fat images can replace T1-weighted spin-echo images. Radiology. 2018;286:948–59.
Park DK, An HS, Lurie JD, et al. Does multilevel lumbar stenosis lead to poorer outcomes?: a subanalysis of the spine patient outcomes research trial (SPORT) lumbar stenosis study. Spine (Phila Pa 1976). 2010;35:439–46.
Weinert AM Jr, Rizzo TD Jr. Nonoperative management of multilevel lumbar disk herniations in an adolescent athlete. Mayo Clin Proc. 1992;67:137–41.
D'Hooge R, Cagnie B, Crombez G, Vanderstraeten G, Dolphens M, Danneels L. Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther. 2012;17:584–8.
Lee JC, Cha JG, Kim Y, Kim YI, Shin BJ. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: comparison with the normal controls. Spine (Phila Pa 1976). 2008;33:318–25.
Cassidy FH, Yokoo T, Aganovic L, et al. Fatty liver disease: MR imaging techniques for the detection and quantification of liver steatosis. Radiographics. 2009;29:231–60.
Kjaer P, Bendix T, Sorensen JS, Korsholm L, Leboeuf-Yde C. Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain. BMC Med. 2007;5:2.
Nakagaki K, Ozaki J, Tomita Y, Tamai S. Fatty degeneration in the supraspinatus muscle after rotator cuff tear. J Shoulder Elb Surg. 1996;5:194–200.
Nozaki T, Tasaki A, Horiuchi S, et al. Quantification of fatty degeneration within the supraspinatus muscle by using a 2-point Dixon method on 3-T MRI. AJR Am J Roentgenol. 2015;205:116–22.
Fischer MA, Pfirrmann CW, Espinosa N, Raptis DA, Buck FM. Dixon-based MRI for assessment of muscle-fat content in phantoms, healthy volunteers and patients with achillodynia: comparison to visual assessment of calf muscle quality. Eur Radiol. 2014;24:1366–75.
Schlaeger S, Klupp E, Weidlich D, et al. T2-weighted Dixon turbo spin echo for accelerated simultaneous grading of whole-body skeletal muscle fat infiltration and edema in patients with neuromuscular diseases. J Comput Assist Tomogr. 2018;42:574–9.
Karampinos DC, Melkus G, Baum T, Bauer JS, Rummeny EJ, Krug R. Bone marrow fat quantification in the presence of trabecular bone: initial comparison between water-fat imaging and single-voxel MRS. Magn Reson Med. 2014;71:1158–65.
Elliott J, Pedler A, Kenardy J, Galloway G, Jull G, Sterling M. The temporal development of fatty infiltrates in the neck muscles following whiplash injury: an association with pain and posttraumatic stress. PLoS One. 2011;6:e21194.
Fortin M, Videman T, Gibbons LE, Battie MC. Paraspinal muscle morphology and composition: a 15-yr longitudinal magnetic resonance imaging study. Med Sci Sports Exerc. 2014;46:893–901.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
1) This manuscript has been submitted to Skeletal Radiology alone, at this time.
2) This manuscript has not previously been published.
3) This study was not split up into several parts to increase the quantity of submissions.
4) No data have been fabricated or manipulated.
5) No data, text, or theories by others are presented as if they were the author’s own. Proper acknowledgements to other works have been given, quotation marks were used for verbatim copying of material, and permissions were secured for material that is copyrighted.
6) Authors whose names appear on the submission have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results.
7) Authors are prepared to send documentation or data in order to verify the validity of their results.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval and informed consent
The institutional review board approved this retrospective study and the informed consent was waived.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, S.K., Jung, JY., Kang, Y.R. et al. Fat quantification of multifidus muscle using T2-weighted Dixon: which measurement methods are best suited for revealing the relationship between fat infiltration and herniated nucleus pulposus. Skeletal Radiol 49, 263–271 (2020). https://doi.org/10.1007/s00256-019-03270-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03270-5