Abstract
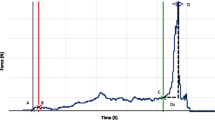
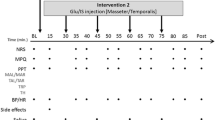
The aim of the experiment was to test the hypothesis that experimental pain in the masseter muscle or temporomandibular joint (TMJ) would perturb the oral fine motor control, reflected in bigger variability of bite force values and jaw muscle activity, during repeated splitting of food morsels. Twenty healthy volunteers participated in four sessions. An intervention was made by injection of either 0.2 ml of monosodium glutamate/isotonic saline (MSG/IS) (randomized) in either the masseter or TMJ (randomized). The participants were asked to hold and split a flat-faced placebo tablet with their anterior teeth, thirty times each at baseline, during intervention and post-intervention. Pain was measured using a 0–10 visual analog scale. The force applied by the teeth to “hold” and “split” the tablet along with the corresponding electromyographic (EMG) activity of the jaw muscles and subject-based reports on perception of pain was recorded. The data analysis included a three-way analysis of variance model. The peak pain intensity was significantly higher during the painful MSG injections in the TMJ (6.1 ± 0.4) than the injections in masseter muscle (5.5 ± 0.5) (P = 0.037). Variability of hold force was significantly smaller during the MSG injection than IS injection in the masseter (P = 0.024). However, there was no significant effect of intervention on the variability of split force during the masseter injections (P = 0.769) and variability of hold and split force during the TMJ injections (P = 0.481, P = 0.545). The variability of the EMG activity of the jaw muscles did not show significant effects of intervention. Subject-based reports revealed that pain did not interfere in the ability to hold the tablet in 57.9 and 78.9 %, and the ability to split the tablet in 78.9 and 68.4 %, of the participants, respectively, during painful masseter and TMJ injections. Hence, experimental pain in the masseter muscle or TMJ did not have any robust effect in terms of bigger variability of bite force and jaw muscle activity, during repeated splitting of food morsels.




Similar content being viewed by others
References
Akhter R, Benson J, Svensson P, Nicholas MK, Peck CC, Murray GM (2014) Experimental jaw muscle pain increases pain scores and jaw movement variability in higher pain catastrophizers. J Oral Facial Pain Headache 28:191–1204. doi:10.11607/ofph.1211
Alstergren P, Ernberg M, Nilsson M, Hajati AK, Sessle BJ, Kopp S (2010) Glutamate-induced temporomandibular joint pain in healthy individuals is partially mediated by peripheral NMDA receptors. J Orofac Pain 24:172–180
Blanksma NG, van Eijden TM (1995) Electromyographic heterogeneity in the human temporalis and masseter muscles during static biting, open/close excursions, and chewing. J Dent Res 74:1318–1327
Cairns BE, Sessle BJ, Hu JW (1998) Evidence that excitatory amino acid receptors within the temporomandibular joint region are involved in the reflex activation of the jaw muscles. J Neurosci 18:8056–8064
Castrillon EE, Cairns BE, Wang K, Arendt-Nielsen L, Svensson P (2012) Comparison of glutamate-evoked pain between the temporalis and masseter muscles in men and women. Pain 153:823–829. doi:10.1016/j.pain.2012.01.003
Cavanagh PR, Komi PV (1979) Electromechanical delay in human skeletal muscle under concentric and eccentric contractions. Eur J Appl Physiol Occup Physiol 42:159–163
Coghill RC (2010) Individual differences in the subjective experience of pain: new insights into mechanisms and models. Headache 50:1531–1535. doi:10.1111/j.1526-4610.2010.01763.x
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6:301–355
Fukuda EJ, Pompeu JE, Lucareli PRG, Garbelotti S, Gimenes RO, Apolinário A (2010) Root mean square value of the electromyographic signal in the isometric torque of the quadriceps, hamstrings and brachial biceps muscles in female subjects. J Appl Res 10:32–39
Hannam AG, McMillan AS (1994) Internal organization in the human jaw muscles. Crit Rev Oral Biol Med 5:55–89
Hasenbring M (2000) Attentional control of pain and the process of chronification. Prog Brain Res 129:525–534. doi:10.1016/s0079-6123(00)29038-9
Hasenbring MI, Verbunt JA (2010) Fear-avoidance and endurance-related responses to pain: new models of behavior and their consequences for clinical practice. Clin J Pain 26:747–753. doi:10.1097/AJP.0b013e3181e104f2
Iida T, Komiyama O, Obara R, Baad-Hansen L, Kawara M, Svensson P (2013) Influence of visual feedback on force-EMG curves from spinally innervated versus trigeminally innervated muscles. Arch Oral Biol 58:331–339. doi:10.1016/j.archoralbio.2012.12.005
Kumar A, Svensson KG, Baad-Hansen L, Trulsson M, Isidor F, Svensson P (2014) Optimization of jaw muscle activity and fine motor control during repeated biting tasks. Arch Oral Biol 59:1342–1351. doi:10.1016/j.archoralbio.2014.08.009
Kumar A, Castrillon E, Svensson P (2015) Can experimentally evoked pain in the jaw muscles or temporomandibular joint affect anterior bite force in humans? J Oral Facial Pain Headache 29:31–40. doi:10.11607/ofph.1268
Lindroth JE, Schmidt JE, Carlson CR (2002) A comparison between masticatory muscle pain patients and intracapsular pain patients on behavioral and psychosocial domains. J Orofac Pain 16:277–283
List T, Tegelberg A, Haraldson T, Isacsson G (2001) Intra-articular morphine as analgesic in temporomandibular joint arthralgia/osteoarthritis. Pain 94:275–282
Loeser JD, Melzack R (1999) Pain: an overview. The Lancet 353:1607–1609. doi:10.1016/S0140-6736(99)01311-2
Lund JP (1991) Mastication and its control by the brain stem. Crit Rev Oral Biol Med 2:33–64
Lund JP, Kolta A (2006) Generation of the central masticatory pattern and its modification by sensory feedback. Dysphagia 21:167–174. doi:10.1007/s00455-006-9027-6
Lund JP, Donga R, Widmer CG, Stohler CS (1991) The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol 69:683–694
McCaul KD, Malott JM (1984) Distraction and coping with pain. Psychol Bull 95:516–533
McCreary CP, Clark GT, Merril RL, Flack V, Oakley ME (1991) Psychological distress and diagnostic subgroups of temporomandibular disorder patients. Pain 44:29–34
Melzack R (1975) The McGill Pain Questionnaire: major properties and scoring methods. Pain 1:277–299
Murray GM, Peck CC (2007) Orofacial pain and jaw muscle activity: a new model. J Orofac Pain 21:263–278 (discussion 279–288)
Nakamura Y, Katakura N (1995) Generation of masticatory rhythm in the brainstem. Neurosci Res 23:1–19
Peck CC, Murray GM, Gerzina TM (2008) How does pain affect jaw muscle activity? The Integrated Pain Adaptation Model. Aust Dent J 53:201–207. doi:10.1111/j.1834-7819.2008.00050.x
Peck CC, Wirianski A, Murray GM (2010) Jaw motor plasticity in health and disease. Comput Methods Biomech Biomed Eng 13:455–458. doi:10.1080/10255840903453090
Pratt CA, Loeb GE (1991) Functionally complex muscles of the cat hindlimb. I. Patterns of activation across sartorius. Exp Brain Res 85:243–256
Quartana PJ, Campbell CM, Edwards RR (2009) Pain catastrophizing: a critical review. Expert Rev Neurother 9:745–758. doi:10.1586/ern.09.34
Ro JY, Svensson P, Capra N (2002) Effects of experimental muscle pain on electromyographic activity of masticatory muscles in the rat. Muscle Nerve 25:576–584
Rudy TE, Turk DC, Kubinski JA, Zaki HS (1995) Differential treatment responses of TMD patients as a function of psychological characteristics. Pain 61:103–112
Sae-Lee D, Whittle T, Forte AR, Peck CC, Byth K, Sessle BJ, Murray GM (2008a) Effects of experimental pain on jaw muscle activity during goal-directed jaw movements in humans. Exp Brain Res 189:451–462. doi:10.1007/s00221-008-1439-0
Sae-Lee D, Whittle T, Peck CC, Forte AR, Klineberg IJ, Murray GM (2008b) Experimental jaw-muscle pain has a differential effect on different jaw movement tasks. J Orofac Pain 22:15–29
Sarlani E, Grace EG, Reynolds MA, Greenspan JD (2004) Evidence for up-regulated central nociceptive processing in patients with masticatory myofascial pain. J Orofac Pain 18:41–55
Sessle B, Avivi-Arber L, Murray G (2013) Motor Control of Masticatory Muscles. In: McLoon LK, Andrade F (eds) Craniofacial muscles. Springer, New York, pp 111–130
Shiau YY, Peng CC, Wen SC, Lin LD, Wang JS, Lou KL (2003) The effects of masseter muscle pain on biting performance. J Oral Rehabil 30:978–984
Shida T, Abe S, Sakiyama K, Agematsu H, Mitarashi S, Tamatsu Y, Ide Y (2005) Superficial and deep layer muscle fibre properties of the mouse masseter before and after weaning. Arch Oral Biol 50:65–71. doi:10.1016/j.archoralbio.2004.08.005
Shimada A, Hara S, Svensson P (2013) Effect of experimental jaw muscle pain on EMG activity and bite force distribution at different level of clenching. J Oral Rehabil 40:826–833. doi:10.1111/joor.12096
Smith R, Pearce SL, Miles TS (2006) Experimental muscle pain does not affect fine motor control of the human hand. Exp Brain Res 174:397–402. doi:10.1007/s00221-006-0474-y
Soboleva U, Laurina L, Slaidina A (2005) The masticatory system—an overview. Stomatologija 7:77–80
Stohler CS, Ashton-Miller JA, Carlson DS (1988) The effects of pain from the mandibular joint and muscles on masticatory motor behaviour in man. Arch Oral Biol 33:175–182
Sullivan BS, Pivik J (1995) The Pain Catastrophizing Scale: development and validation. Psychol Assess 432–524
Svensson P (2007) What can human experimental pain models teach us about clinical TMD? Arch Oral Biol 52:391–394. doi:10.1016/j.archoralbio.2006.11.015
Svensson P, Graven-Nielsen T (2001) Craniofacial muscle pain: review of mechanisms and clinical manifestations. J Orofac Pain 15:117–145
Svensson KG, Trulsson M (2009) Regulation of bite force increase during splitting of food. Eur J Oral Sci 117:704–710. doi:10.1111/j.1600-0722.2009.00691.x
Svensson KG, Trulsson M (2011) Impaired force control during food holding and biting in subjects with tooth- or implant-supported fixed prostheses. J Clin Periodontol 38:1137–1146. doi:10.1111/j.1600-051X.2011.01781.x
Svensson P, Arendt-Nielsen L, Houe L (1996) Sensory-motor interactions of human experimental unilateral jaw muscle pain: a quantitative analysis. Pain 64:241–249
Svensson P, Houe L, Arendt-Nielsen L (1997) Bilateral experimental muscle pain changes electromyographic activity of human jaw-closing muscles during mastication. Exp Brain Res 116:182–185
Svensson P, Arendt-Nielsen L, Houe L (1998) Muscle pain modulates mastication: an experimental study in humans. J Orofac Pain 12:7–16
Trulsson M (2006) Sensory-motor function of human periodontal mechanoreceptors. J Oral Rehabil 33:262–273. doi:10.1111/j.1365-2842.2006.01629.x
Trulsson M, Gunne HS (1998) Food-holding and -biting behavior in human subjects lacking periodontal receptors. J Dent Res 77:574–582
Trulsson M, Johansson RS (1996) Forces applied by the incisors and roles of periodontal afferents during food-holding and -biting tasks. Exp Brain Res 107:486–496
Trulsson M, Johansson RS, Olsson KA (1992) Directional sensitivity of human periodontal mechanoreceptive afferents to forces applied to the teeth. J Physiol 447:373–389
Turker KS, Johnsen SE, Sowman PF, Trulsson M (2006) A study on synaptic coupling between single orofacial mechanoreceptors and human masseter muscle. Exp Brain Res 170:488–500. doi:10.1007/s00221-005-0231-7
Widmalm SE, Lillie JH, Ash MM Jr (1988) Anatomical and electromyographic studies of the digastric muscle. J Oral Rehabil 15:3–21
Wright EF (2000) Referred craniofacial pain patterns in patients with temporomandibular disorder. J Am Dent Assoc 131:1307–1315
Yu XM, Sessle BJ, Vernon H, Hu JW (1995) Effects of inflammatory irritant application to the rat temporomandibular joint on jaw and neck muscle activity. Pain 60:143–149
Acknowledgments
This study was funded by the Section of Orofacial Pain and Jaw Function, Department of Dentistry, Aarhus University and the Danish Dental Association, Denmark.
Conflict of interest
None.
Ethical standard
Informed consent was obtained from all the participants prior to their participation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, A., Castrillon, E., Svensson, K.G. et al. Effects of experimental craniofacial pain on fine jaw motor control: a placebo-controlled double-blinded study. Exp Brain Res 233, 1745–1759 (2015). https://doi.org/10.1007/s00221-015-4245-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-015-4245-5