Abstract
Introduction and hypothesis
We evaluated patients’ perception and satisfaction with nonsurgical pulsed magnetic stimulation (PMS) for treatment of female stress urinary incontinence (SUI) in a randomized, double-blind, sham-controlled trial.
Methods
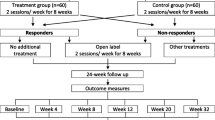
Women with SUI (n = 120) were randomized to either active or sham PMS for 8 weeks (twice/week). Patients answered seven questions on their perception and acceptability, each measured on a 5-point Likert scale. Treatment satisfaction was assessed using two parameters: (i) the single-item question “Overall, please rate how satisfied you are with the treatment” and (ii) Patient Global Impression of Improvement (PGI-I). All adverse events were documented.
Results
A total of 115 patients completed treatments (active: n = 57, sham: n = 58). There were no significant differences between groups in all parameters regarding perception and acceptability (p > 0.05). In terms of treatment satisfaction, a significantly higher proportion of patients in the active group (n = 47/57, 82.4%) were either mostly or completely satisfied compared with those in the sham group (n = 27/58, 46.6%) ((p = 0.001). Similarly, a statistically significantly higher percentage of patients in the active group (n = 39/57, 68.4%) felt much or very much better compared with patients in the sham group (n = 11/58, 19.0%) as measured using the PGI-I (p < 0.001). Three (5.3%) patients in the active group and five (8.6%) in the sham group experienced adverse events (p = 0.72). Regardless of treatment arms, 109 (94.8%) patients would not consider surgical options even if they required further treatment for their condition.
Conclusion
PMS was well accepted, well tolerated, and resulted in a high treatment satisfaction among women with SUI.

Similar content being viewed by others
References
Payne CK. Conservative Management of Urinary Incontinence: Behavioral and pelvic floor therapy, urethral and pelvic devices. In: McDougal WS, Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peter CA, Ramchandani P, editors. Campbell Walsh urology. 10th ed. Philadelphia: W.B. Saunders; 2012. p. 2003–25. doi:10.1016/b978-1-4160-6911-9.00069-4.
Abrams P, Cardozo L, Wein A, Wagg A. Incontinence: 6th International Consultation on Incontinence, Tokyo, September 2016. ICUD, 6th ed.; 2017.
Lim R, Liong ML, Leong WS, Khan NAK, Yuen KH. Effect of stress urinary incontinence on sexual function of couples and quality of life of the patients. J Urol. 2016; doi:10.1016/j.juro.2016.01.090.
Dumoulin C, Hay-Smith J, Habée-Séguin GM, Mercier J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: a short version Cochrane systematic review with meta-analysis. Neurourol Urodyn. 2015;34(4):300–8. doi:10.1002/nau.22700.
Lipp A, Shaw C, Glavind K. Mechanical devices for urinary incontinence in women. Cochrane Database Syst Rev. 2011;7:CD001756. doi:10.1002/14651858.CD001756.pub5.
Herbison GP, Dean N. Weighted vaginal cones for urinary incontinence. Cochrane Database Syst Rev. 2013;7:CD002114. doi:10.1002/14651858.CD002114.pub2.
Ford Abigail A, Rogerson L, Cody June D, Ogah J. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2015;7:CD006375. doi:10.1002/14651858.CD006375.pub3.
Diokno A, Yuhico M Jr. Preference, compliance and initial outcome of therapeutic options chosen by female patients with urinary incontinence. J Urol. 1995;154(5):1727–31.
Karantanis E, Parsons M, Blackwell A, Robinson D, Cardozo L, Moore KH, et al. Women’s treatment preferences for stress urinary incontinence-physiotherapy or surgery. Aust N Z Continence J. 2014;20(2):34–6. 38-40, 42
Paddison K. Complying with pelvic floor exercises: a literature review. Nurs Stand. 2002;16(39):33–8. doi:10.7748/ns2002.06.16.39.33.c3209.
Frawley HC, McClurg D, Mahfooza A, Hay-Smith J, Dumoulin C. Health professionals’ and patients’ perspectives on pelvic floor muscle training adherence—2011 ICS state-of-the-science seminar research paper IV of IV. Neurourol Urodyn. 2015;34(7):632–9. doi:10.1002/nau.22774.
Schreiner L, dos Santos TG, de Souza ABA, Nygaard CC, da Silva Filho IG. Electrical stimulation for urinary incontinence in women: a systematic review. Int Braz J Urol. 2013;39(4):454–64.
Markov MS. Pulsed electromagnetic field therapy history, state of the art and future. Environmentalist. 2007;27(4):465–75. doi:10.1007/s10669-007-9128-2.
Bickford RG, Fremming B. Neuronal stimulation by pulsed magnetic fields in animals and man. In: Digest of the 6th Internat. Conf. Medical Electronics and Biological Engineering; 1965. p. 112.
Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlan SJ. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology. 1999;53(6):1108–11.
Lim R, Liong ML, Leong WS, Khan NAK, Yuen KH. Randomized controlled trial of pulsed magnetic stimulation for stress urinary incontinence: 1-year results. J Urol. 2017;197(5):1302–8. doi:10.1016/j.juro.2016.11.091.
Lim R, Lee SWH, Tan PY, Liong ML, Yuen KH. Efficacy of electromagnetic therapy for urinary incontinence: a systematic review. Neurourol Urodyn. 2015;34(8):713–22. doi:10.1002/nau.22672.
Lim R, Liong ML, Leong WS, Khan NAK, Yuen KH. Magnetic stimulation for stress urinary incontinence: study protocol for a randomized controlled trial. Trials. 2015;16:279. doi:10.1186/s13063-015-0803-1.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. doi:10.1002/nau.20798.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30. doi:10.1002/nau.20041.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Wright P, Haybittle J. Design of forms for clinical trials (1). Br Med J. 1979;2(6189):529–30.
Wright P, Haybittle J. Design of forms for clinical trials (2). Br Med J. 1979;2(6190):590–2.
Wright P, Haybittle J. Design of forms for clinical trials (3). Br Med J. 1979;2(6191):650–1.
Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22:140.
Yalcin I, Bump RC. Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol. 2003;189(1):98–101. doi:10.1067/mob.2003.379.
Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlin SJ. Update on extracorporeal magnetic innervation (EXMI) therapy for stress urinary incontinence. Urology. 2000;56(6 Suppl 1):82–6.
Fujishiro T, Enomoto H, Ugawa Y, Takahashi S, Ueno S, Kitamura T. Magnetic stimulation of the sacral roots for the treatment of stress incontinence: an investigational study and placebo controlled trial. J Urol. 2000;164(4):1277–9.
Yamanishi T, Yasuda K, Suda S, Ishikawa N, Sakakibara R, Hattori T. Effect of functional continuous magnetic stimulation for urinary incontinence. J Urol. 2000;163(2):456–9.
Yokoyama T, Fujita O, Nishiguchi J, Nozaki K, Nose H, Inoue M, et al. Extracorporeal magnetic innervation treatment for urinary incontinence. Int J Urol. 2004;11(8):602–6. doi:10.1111/j.1442-2042.2004.00857.x.
Lee JSHJY, Kim MH, Seo JT. Comparative study of the pelvic floor magnetic stimulation with BIOCON-2000TM in female urinary incontinence patients. Korean J Urol. 2004;45(5):438–43.
Unsal A, Saglam R, Cimentepe E. Extracorporeal magnetic stimulation for the treatment of stress and urge incontinence in women--results of 1-year follow-up. Scand J Urol Nephrol. 2003;37(5):424–8. doi:10.1080/00365590310021258.
Bakar Y, Cinar Ozdemir O, Ozengin N, Duran B. The use of extracorporeal magnetic innervation for the treatment of stress urinary incontinence in older women: a pilot study. Arch Gynecol Obstet. 2011;284(5):1163–8. doi:10.1007/s00404-010-1814-5.
Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, et al. Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med. 2013;369(12):1124–33. doi:10.1056/NEJMoa1210627.
Richter HE, Burgio KL, Brubaker L, Nygaard IE, Ye W, Weidner A, et al. Continence Pessary compared with Behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115(3):609–17. doi:10.1097/AOG.0b013e3181d055d4.
Acknowledgements
We thank all study participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was partially funded by QRS International.
Conflicts of interest
RL was a full-time doctoral student at Universiti Sains Malaysia who received a research assistant allowance from QRS International during the study period. All other authors declare that they have no conflict of interest.
Ethical committee
The study was approved by the Joint Ethics Committee of the School of Pharmaceutical Sciences, USM-HLWE on Clinical Studies (USM-HLWE/IEC/2013[0006]).
Rights and permissions
About this article
Cite this article
Lim, R., Liong, M.L., Leong, W.S. et al. Patients’ perception and satisfaction with pulsed magnetic stimulation for treatment of female stress urinary incontinence. Int Urogynecol J 29, 997–1004 (2018). https://doi.org/10.1007/s00192-017-3425-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3425-1