Abstract
Objective
Brevity is critical to the broad adoption of any screening measure. We examine the efficacy of a short Conners Continuous Performance Test (CCPT 3) to screen for concussion symptoms.
Method
Data were from 20 U.S. sites, including university/schools conducting baseline testing (N = 817) and post-concussion assessments in medical settings (N = 108) from March 2018 to March 2020. Nine hundred twenty-five participants (57.3% female) aged 8–66 (M = 19.4, SD = 6.1) completed the computerized CCPT 3, Balance Error Scoring System, NIH 4-meter gait test, and 31-item Centers for Disease Control and Prevention (CDC) concussion symptom checklist.
Results
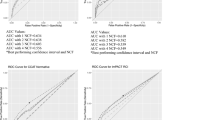
Short CCPT 3 scores correlate highly with full CCPT 3, with coefficients of .70–.96 (M = .88). Short CCPT 3 explains 16.8% variance in CDC concussion symptoms (F(8, 910) = 23.01, p < .001; Cohen’s d = .90) and provides incremental validity (15% variance; d = .78) over behavioral measures (Fchange (8, 842) = 20.11, p < .001). Predictive validity of the short CCPT 3 was greater for those having a recent concussion (22.1% variance, d = 1.07; F(8, 97) = 3.45, p= .002). Scores also predict concussion history.
Conclusions
The short CCPT 3 yields large effect sizes when predicting CDC concussion symptoms, compares favorably to other concussion measures, and shows no trade-off from the full CCPT, which has previously predicted concussion symptoms and severity. Short CCPT 3 scores can objectively quantify cognitive functioning to serve as a screener and inform return-to-play decisions even for post-acute presentations in children, adolescents, and adults.
Similar content being viewed by others
References
Alsalaheen, B., Stockdale, K., Pechumer, D., Broglio, S. P., & Marchetti, G. F. (2017). A comparative meta-analysis of the effects of concussion on a computerized neurocognitive test and self-reported symptoms. Journal of Athletic Training, 52(9), 834–846. https://doi.org/10.4085/1062-6050-52.7.05.
Belanger, H. G., & Vanderploeg, R. D. (2005). The neuropsychological impact of sports-related concussion: A meta-analysis. Journal of the International Neuropsychological Society, 11(4), 345–357. https://doi.org/10.1017/s1355617705050411.
Bergemalm, P. O., & Lyxell, B. (2005). Appearances are deceptive? Long-term cognitive and central auditory sequelae from closed head injury. International Journal of Audiology, 44(1), 39–44. https://doi.org/10.1080/14992020400022546.
Broglio, S. P., & Puetz, T. W. (2008). The effect of sport concussion on neurocognitive function, self-report symptoms and postural control: A meta-analysis. Sports Medicine, 38(1), 53–67. https://doi.org/10.2165/00007256-200838010-00005.
Broglio, S. P., Ferrara, M. S., Macciocchi, S. N., Baumgartner, T. A., & Elliott, R. (2007). Test–retest reliability of computerized concussion assessment programs. Journal of Athletic Training, 42(4), 509–514.
Brooks, B. L., Silverberg, N., Maxwell, B., Mannix, R., Zafonte, R., Berkner, P. D., & Iverson, G. L. (2018). Investigating effects of sex differences and prior concussions on symptom reporting and cognition among adolescent soccer players. The American Journal of Sports Medicine, 46(4), 961–968. https://doi.org/10.1177/0363546517749588.
Centers for Disease Control and Prevention. (2003). National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Centers for Disease Control and Prevention; Atlanta, GA, USA.
Centers for Disease Control and Prevention. (2015). Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention. Atlanta, GA.
Centers for Disease Control and Prevention (retrieved 2020). Heads up concussion in high school sports: Guide for coaches. www.cdc.gov/headsup/pdfs/highschoolsports/coach_guide-a.pdf
Chen, H., Koh, C., Hsieh, C., & Hsueh, I. (2009). Test–re-test reliability of two sustained attention tests in persons with chronic stroke. Brain Injury, 23(9), 715–722. https://doi.org/10.1080/02699050903013602.
Chen, K., Lin, G., Chen, N., Wang, J., & Hsieh, C. (2020). Practice effects and test-retest reliability of the Continuous Performance Test, identical pairs version in patients with schizophrenia over four serial assessments. Archives of Clinical Neuropsychology, 35(5), 545–552. https://doi.org/10.1093/arclin/acaa004.
Chin, E. Y., Nelson, L. D., Barr, W. B., McCrory, P., & McCrea, M. A. (2016). Reliability and validity of the Sport Concussion Assessment Tool–3 (SCAT3) in high school and collegiate athletes. The American Journal of Sports Medicine, 44(9), 2276–2285. https://doi.org/10.1177/0363546516648141.
Coldren, R. L., Kelly, M. P., Parish, R. V., Dretsch, M., & Russell, M. L. (2010). Evaluation of the military acute concussion evaluation for use in combat operations more than 12 hours after injury. Military Medicine, 175(7), 477–481. https://doi.org/10.7205/milmed-d-09-00258.
Collins, M. W., Kontos, A. P., Okonkwo, D. O., Almquist, J., Bailes, J., Barisa, M., et al. (2016). Statements of agreement from the Targeted Evaluation and Active Management (TEAM) approaches to treating concussion meeting held in Pittsburgh, October 15-16, 2015. Neurosurgery, 79(6), 912–929. https://doi.org/10.1227/NEU.0000000000001447.
Conners, C. K. (1995). Conners’ continuous performance test computer program: User’s manual. Multi-Health Systems.
Conners, C. K. (2014). Conners’ Continuous Performance Test (3rd ed.). Multi-Health Systems Inc..
Daneshvar, D. H., Nowinski, C. J., McKee, A. C., & Cantu, R. C. (2011). The epidemiology of sport-related concussion. Clinics in Sports Medicine, 30(1), 1–vii. https://doi.org/10.1016/j.csm.2010.08.006.
Defense and Veterans Brain Injury Center. (2019). Appendix G: MACE 2: Military Acute Concussion Evaluation. In National Academies of Sciences, Engineering, and Medicine, Evaluation of the disability determination process for traumatic brain injury in veterans (pp. 137-143). The National Academies Press. 10.17226/25317
Echemendia, R. J., Broglio, S. P., Davis, G. A., Guskiewicz, K. M., Hayden, K. A., Leddy, J. J., et al. (2017a). What tests and measures should be added to the SCAT3 and related tests to improve their reliability, sensitivity and/or specificity in sideline concussion diagnosis? A systematic review. British Journal of Sports Medicine, 51(11), 895–901. https://doi.org/10.1136/bjsports-2016-097466.
Echemendia, R. J., Meeuwisse, W., McCrory, P., Davis, G. A., Putukian, M., Leddy, J., Makdissi, M., Sullivan, S. J., Broglio, S. P., Raftery, M., Schneider, K., Kissick, J., McCrea, M., Dvořák, J., Sills, A. K., Aubry, M., Engebretsen, L., Loosemore, M., Fuller, G., Kutcher, J., et al. (2017b). The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. British Journal of Sports Medicine, 51(11), 848–850. https://doi.org/10.1136/bjsports-2017-097506.
Eisenberg, M. A., Andrea, J., Meehan, W., & Mannix, R. (2013). Time interval between concussions and symptom duration. Pediatrics, 132, 8–17.
Farnsworth, J. L., Dargo, L., Ragan, B. G., & Kang, M. (2017). Reliability of computerized neurocognitive tests for concussion assessment: A meta-analysis. Journal of Athletic Training, 52(9), 826–833. https://doi.org/10.4085/1062-6050-52.6.03.
Galbiati, S., Recla, M., Pastore, V., Liscio, M., Bardoni, A., Castelli, E., & Strazzer, S. (2009). Attention remediation following traumatic brain injury in childhood and adolescence. Neuropsychology, 23(1), 40–49. https://doi.org/10.1037/a0013409.
Gale, S. D., Baxter, L., Roundy, N., & Johnson, S. C. (2005). Traumatic brain injury and grey matter concentration: A preliminary voxel based morphometry study. Journal of Neurology, Neurosurgery and Psychiatry, 76(7), 984–988. https://doi.org/10.1136/jnnp.2004.036210.
Gibson, D. B. (2015). Effect size as the essential statistic in developing methods for mTBI diagnosis. Frontiers in Neurology, 6, 126. https://doi.org/10.3389/fneur.2015.00126.
Halterman, C. I., Langan, J., Drew, A., Rodriguez, E., Osternig, L. R., Chou, L. S., & van Donkelaar, P. (2006). Tracking the recovery of visuospatial attention deficits in mild traumatic brain injury. Brain, 129(Pt 3), 747–753. https://doi.org/10.1093/brain/awh705.
Houston, M. N., Van Pelt, K. L., D’Lauro, C., Brodeur, R. M., Campbell, D. E., McGinty, G. T., et al. (2020). Test-Retest reliability of concussion baseline assessments in United States Service Academy Cadets: A report from the National Collegiate Athletic Association (NCAA) - Department of Defense (DoD) CARE Consortium. Journal of the International Neuropsychological Society, 16, 1–12. https://doi.org/10.1017/S1355617720000594.
Hunt, T. N., Ferrara, M. S., Miller, L. S., & Macciocchi, S. (2007). The effect of effort on baseline neuropsychological test scores in high school football athletes. Archives of Clinical Neuropsychology, 22, 615–621.
Iverson, G. L., Lovell, M. R., & Collins, M. W. (2003). Interpreting change on ImPACT following sport concussion. The Clinical Neuropsychologist, 17(4), 460–467. https://doi.org/10.1076/clin.17.4.460.27934.
Kamins, J., Bigler, E., Covassin, T., Henry, L., Kemp, S., Leddy, J. J., et al. (2017). What is the physiological time to recovery after concussion? A systematic review. British Journal of Sports Medicine, 51, 935–940. https://doi.org/10.1136/bjsports-2016-097464.
Keightley, M. L., Yule, A., Garland, K., Reed, N., McAuliffe, J., Garton, J., Green, S., & Taha, T. (2010). Sports-related mild traumatic brain injury in female youths. BMJ Case Reports, 2010. https://doi.org/10.1136/bcr.09.2009.2309.
Keith, J., Williams, M., Taravath, S., & Lecci, L. (2019). A clinician’s guide to machine learning in neuropsychological research and practice. Journal of Pediatric Neuropsychology, 5, 177–187. https://doi.org/10.1007/s40817-019-00075-1.
Kim, E., Lauterbach, E. C., Reeve, A., Arciniegas, D. B., Coburn, K. L., Mendez, M. F., Rummans, T. A., Coffey, E. C., & ANPA Committee on Research. (2007). Neuropsychiatric complications of traumatic brain injury: A critical review of the literature (a report by the ANPA Committee on Research). The Journal of Neuropsychiatry and Clinical Neurosciences, 19(2), 106–127. https://doi.org/10.1176/jnp.2007.19.2.106.
Kirelik, S. B., & McAvoy, K. (2016). Acute concussion management with remove–reduce/educate/adjust–accommodate/pace (REAP). The Journal of Emergency Medicine, 50(2), 320–324. https://doi.org/10.1016/j.jemermed.2015.02.054.
Kontos, A. P., Monti, K., Thomas, E., Holland, C., Thomas, D., Bitzer, H., Mucha, A., & Collins, M. W. (2019). Reliability and factors associated with false positives on the Vestibular/Ocular Motor Screening (VOMS) tool in US military personnel. Archives of Clinical Neuropsychology, 34(5), 762. https://doi.org/10.1093/arclin/acz026.32.
Lange, R. T., Iverson, G. L., Brickell, T. A., Staver, T., Pancholi, S., Bhagwat, A., & French, L. M. (2013). Clinical utility of the Conners’ Continuous Performance Test-II to detect poor effort in U.S. Military personnel following traumatic brain injury. Psychological Assessment, 25(2), 339–352. https://doi.org/10.1037/a0030915.
Langlois, J. A., Rutland-Brown, W., & Wald, M. M. (2006). The epidemiology and impact of traumatic brain injury: A brief overview. The Journal of Head Trauma Rehabilitation, 21, 375–378.
Lau, B., Lovell, M. R., Collins, M. W., & Pardini, J. (2009). Neurocognitive and symptom predictors of recovery in high school athletes. Clinical Journal of Sport Medicine, 19(3), 216–221. https://doi.org/10.1097/JSM.0b013e31819d6edb.
Leahy, A. B., Feudtner, C., & Basch, E. (2018). Symptom monitoring in pediatric oncology using patient-reported outcomes: Why, how, and where next. The Patient, 11(2), 147–153. https://doi.org/10.1007/s40271-017-0279-z.
Lecci, L., Williams, M., Taravath, S., Frank, H. G., Dugan, K., Page, R., & Keith, J. (2020). Validation of a concussion screening battery for use in medical settings: Predicting Centers for Disease Control concussion symptoms in children and adolescents. Archives of Clinical Neuropsychology, 35(3), 265–274. https://doi.org/10.1093/arclin/acz041.
Levan, A., Black, G., Mietchen, J., Baxter, L., Kirwan, C. B., & Gale, S. D. (2015). Right frontal pole cortical thickness and executive functioning in children with traumatic brain injury: The impact on social problems. Brain Imaging and Behavior, 10, 1090–1095. https://doi.org/10.1007/s11682-015-9472-7.
Lippa, S. M. (2018). Performance validity testing in neuropsychology: A clinical guide, critical review, and update on a rapidly evolving literature. The Clinical Neuropsychologist, 32(3), 391–421. https://doi.org/10.1080/13854046.2017.1406146.
Lumba-Brown, A., Teramoto, M., Bloom, O. J., Brody, D., Chesnutt, J., Clugston, J. R., Collins, M., Gioia, G., Kontos, A., Lal, A., Sills, A., & Ghajar, J. (2020). Concussion guidelines step 2: Evidence for subtype classification. Neurosurgery, 86(1), 2–13. https://doi.org/10.1093/neuros/nyz332.
Mathiasen, R., Hogrefe, C., Harland, K., Peterson, A., & Smoot, M. K. (2018). Longitudinal improvement in Balance Error Scoring System Scores among NCAA Division-I football athletes. Journal of Neurotrauma, 35(4). https://doi.org/10.1089/neu.2017.5072.
McCrea, M. (2001). Standardized mental status testing on the sideline after sport-related concussion. Journal of Athletic Training, 36(3), 274–279.
McCrea, M., Guskiewicz, K., Randolph, C., Barr, W. B., Hammeke, T. A., Marshall, S. W., et al. (2013). Incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college athletes. Journal of the International Neuropsychological Society, 19, 22–33.
McCrory, P., Meeuwisse, W. H., Aubry, M., et al. (2013). Consensus statement on concussion in sport: The 4th International Conference on Concussion in Sport held in Zurich, November 2012. British Journal of Sports Medicine, 47, 250–258. https://doi.org/10.1136/bjsports-2013-092313.
McCrory, P., Meeuwisse, W., Dvořák, J., Aubry, M., Bailes, J., Broglio, S., et al. (2017). Consensus statement on concussion in sport - The 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine, 51(11), 838–847. https://doi.org/10.1136/bjsports-2017-097699.
McKay, C. D., Brooks, B. L., Meeuwisse, W. H., Mrazik, M., Jubinville, A. L., & Emery, C. A. (2013). The effect of age, sex, and concussion history on preseason ImPACT values of elite Canadian youth ice hockey players. British Journal of Sports Medicine, 47(5), e1. https://doi.org/10.1136/bjsports-2012-092101.17.
McLeod, T. C. V., Barr, W. B., McCrea, M., & Guskiewicz, K. M. (2006). Psychometric and measurement properties of concussion assessment tools in youth sports. Journal of Athletic Training, 41(4), 399.
Meier, T. B., Brummel, B. J., Singh, R., Nerio, C. J., Polanski, D. W., & Bellgowan, P. S. (2015). The underreporting of self-reported symptoms following sports-related concussion. Journal of Science and Medicine in Sport, 18(5), 507–511. https://doi.org/10.1016/j.jsams.2014.07.008.
Meyer, G. J., Finn, S. E., Eyde, L. D., Kay, G. G., Moreland, K. L., Dies, R. R., Eisman, E. J., Kubiszyn, T. W., & Reed, G. M. (2001). Psychological testing and psychological assessment: A review of evidence and issues. American Psychologist, 56(2), 128–165. https://doi.org/10.1037/0003-066X.56.2.128.
Narayana, P. A., Yu, X., Hasan, K. M., Wilde, E. A., Levin, H. S., Hunter, J. V., et al. (2015). Multi-modal MRI of mild traumatic brain injury. NeuroImage: Clinical, 7, 87–97.
Naunheim, R. S., Matero, D., & Fucetola, R. (2008). Assessment of patients with mild concussion in the emergency department. The Journal of Head Trauma Rehabilitation, 23(2), 116–122. https://doi.org/10.1097/01.htr.0000314530.30401.70.
Paré, N., Rabin, L. A., Fogel, J., & Pépin, M. (2009). Mild traumatic brain injury and its sequelae: Characterisation of divided attention deficits. Neuropsychological Rehabilitation, 19(1), 110–137. https://doi.org/10.1080/09602010802106486.
Parker, T. M., Osternig, L. R., van Donkelaar, P., & Chou, L. S. (2008). Balance control during gait in athletes and non-athletes following concussion. Medical Engineering & Physics, 12, 1360–1368.
Peters, D. M., Fritz, S. L., & Krotish, D. E. (2013). Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. Journal of Geriatric Physical Therapy, 36(1), 24–30.
Prince, C., & Bruhns, M. E. (2017). Evaluation and treatment of mild traumatic brain injury: The role of neuropsychology. Brain Sciences, 7(8), 105. https://doi.org/10.3390/brainsci7080105.
Reuben, D. B., Magasi, S., McCreath, H. E., Bohannon, R. W., Wang, Y. C., Bubela, D. J., Rymer, W. Z., Beaumont, J., Rine, R. M., Lai, J. S., & Gershon, R. C. (2013). Motor assessment using the NIH Toolbox. Neurology, 80(11 Suppl 3), S65–S75. https://doi.org/10.1212/WNL.0b013e3182872e01.
Riemann, B. L., Guskiewicz, K. M., & Shields, E. W. (1999). Relationship between clinical and forceplate measures of postural stability. Journal of Sport Rehabilitation, 8(2), 71–82. https://doi.org/10.1123/jsr.8.2.71.
Roebuck, H., Freigang, C., & Barry, J. G. (2016). Continuous Performance Tasks: Not just about sustaining attention. Journal of Speech, Language, and Hearing Research: JSLHR, 59(3), 501–510. https://doi.org/10.1044/2015_JSLHR-L-15-0068.
Salgado, J. F. (2018). Transforming the area under the normal curve (AUC) into Cohen’s d, Pearson’s rpb, odds-ratio, and natural log odds-ratio: Two conversion tables. European Journal of Psychology Applied to Legal Context, 10, 35–47. https://doi.org/10.5093/ejpalc2018a5.
Sawilowsky, S. S. (2009). New effect size rules of thumb. Journal of Modern Applied Statistical Methods, 8(2), 597–599. https://doi.org/10.22237/jmasm/1257035100.
Schatz, P., & Putz, B. O. (2006). Cross-validation of measures used for computer-based assessment of concussion. Applied Neuropsychology, 13(3), 151–159. https://doi.org/10.1207/s15324826an1303_2.
Schatz, P., Moser, R. S., Covassin, T., & Karpf, R. (2011). Early indicators of enduring symptoms in high school athletes with multiple previous concussions. Neurosurgery, 68(6), 1562–1567. https://doi.org/10.1227/NEU.0b013e31820e382e.
Sitarenios, G. (2019a). Conners CPT 3 short viability analysis technical report. MHS.
Sitarenios, G. (2019b). Conners CPT 3 short: Examining applicability of full version norms to short version technical report. MHS.
Tallberg, P., Råstam, M., Wenhov, L., Eliasson, G., & Gustafsson, P. (2019). Incremental clinical utility of continuous performance tests in childhood ADHD - an evidence-based assessment approach. Scandinavian Journal of Psychology, 60(1), 26–35. https://doi.org/10.1111/sjop.12499.
Taylor, C. A., Bell, J. M., Breiding, M. J., & Xu, L. (2017). Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C.: 2002), 66(9), 1–16. 10.15585/mmwr.ss6609a1
Thomas, D., Coxe, K., Li, H., Pommering, T., Young, J., Smith, G., & Yang, J. (2018). Length of recovery from sports-related concussions in pediatric patients treated at concussion clinics. Clinical Journal of Sport Medicine, 28(1), 56–63. https://doi.org/10.1097/JSM.0000000000000413.
World Health Organization. (2006). Neurological disorders: Public health challenges. In World Health Organization Press. Switzerland.
Yarnold, P. R. (2017). What is optimal data analysis? Optimal Data Analysis, 6(April), 26–42 odajournal.files.wordpress.com/2019/01/v6a7.pdf.
Zane, K. L., Gfeller, J. D., Roskos, P. T., & Bucholz, R. D. (2016). The clinical utility of the Conners’ Continuous Performance Test-II in traumatic brain injury. Archives of Clinical Neuropsychology, 31(8), 996–1005. https://doi.org/10.1093/arclin/acw078.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lecci, L., Freund, C.T., Ayearst, L.E. et al. Validating a Short Conners CPT 3 as a Screener: Predicting Self-reported CDC Concussion Symptoms in Children, Adolescents, and Adults. J Pediatr Neuropsychol 7, 169–181 (2021). https://doi.org/10.1007/s40817-021-00107-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40817-021-00107-9