Abstract
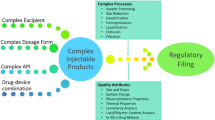
Parenteral delivery is the second leading drug delivery approach after oral delivery. With the current surge of targeted therapeutic (proteins and peptides) and novel formulation approaches, two major sectors of parenteral controlled drug delivery, prolonged release injectables and stimuli-controlled injectables, are projected to grow extensively in the coming two decades as indicated by the current regulatory product approval and industrial pipeline. This chapter discusses these two sectors with details on the impacted therapeutic disease area, potential drug candidates, advancements in manufacturing technologies, and formulation technologies. Moreover, a comprehensive account is also given on the current and next-generation injection devices. Detailed discussions will provide a thorough guide for the development of the parenteral-prolonged and controlled drug delivery systems.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Class S (2004) Health care in focus. Chem Eng News Arch 82(49):18–29. https://doi.org/10.1021/cen-v082n049.p018
Mullin R (2003) Drug development costs about $1.7 billion. Chem Eng News Arch 81(50):8. https://doi.org/10.1021/cen-v081n050.p008a
Bekryl Market Analysts. Global sterile injectable market size analysis, 2018–2028. April 2018.
World Drug Report 2016 (2016) Chapter I Illicit drug markets: situation and trends. United Nations Office on Drugs and Crime. https://www.unodc.org/doc/wdr2016/WORLD_DRUG_REPORT_2016_web.pdf. Accessed 22 Oct 2018
Baser O, Chalk M, Fiellin DA, Gastfriend DR (2011) Cost and utilization outcomes of opioid-dependence treatments. Am J Manag Care 17(Suppl 8):S235–S248
Global status report on alcohol and health (2018) World Health Organization. Sept 2018. http://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1. Accessed 23 Oct 2018.
Weinstein AM, Gorelick DA (2011) Pharmacological treatment of cannabis dependence. Curr Pharm Des 17(14):1351–1358
Dolgin E (2018) What legal weed in Canada means for science. Nature 562(7727):327–330. https://doi.org/10.1038/d41586-018-07037-1
Allsop DJ, Copeland J, Lintzeris N, Dunlop AJ, Montebello M, Sadler C et al (2014) Nabiximols as an agonist replacement therapy during cannabis withdrawal: a randomized clinical trial. JAMA Psychiat 71(3):281–291. https://doi.org/10.1001/jamapsychiatry.2013.3947
Lung Cancer Prevention and Early Detection – Lung Cancer Risk Factors. American Cancer Society. Feb 2016. https://www.cancer.org/cancer/lung-cancer/prevention-and-early-detection/risk-factors.html. Accessed 22 Oct 2018
Health Risks of Smokeless Tobacco. American Cancer Society. Nov 2015. https://www.cancer.org/cancer/cancer-causes/tobacco-and-cancer/smokeless-tobacco.html#references. Accessed 22 Oct 2018
Nicotine Replacement Therapy for Quitting Tobacco. American Cancer Society. Jan 2017. https://www.cancer.org/healthy/stay-away-from-tobacco/guide-quitting-smoking/nicotine-replacement-therapy.html. Accessed 22 Oct 2018
Cahill K, Lindson-Hawley N, Thomas KH, Fanshawe TR, Lancaster T (2016) Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 5:CD006103. https://doi.org/10.1002/14651858.CD006103.pub7
McDonough M (2015) Update on medicines for smoking cessation. Aust Prescr 38(4):106–111
Kerrigan D, Mantsios A, Gorgolas M, Montes M-L, Pulido F, Brinson C et al (2018) Experiences with long acting injectable ART: a qualitative study among PLHIV participating in a phase II study of cabotegravir + rilpivirine (LATTE-2) in the United States and Spain. PLoS One 13(1):e0190487. https://doi.org/10.1371/journal.pone.0190487
A phase 2b/3 double blind safety and efficacy study of injectable cabotegravir compared to daily oral tenofovir disoproxil fumarate/emtricitabine (TDF/FTC), for pre-exposure prophylaxis in HIV-uninfected cisgender men and transgender women who have sex with men. ClinicalTrials.gov 2016. https://www.clinicaltrials.gov/ct2/show/NCT02720094?term=NCT02720094&rank=1
A phase IIa study to evaluate the safety, tolerability and pharmacokinetics of the investigational injectable HIV integrase inhibitor, GSK1265744, in HIV-uninfected men and women. ClinicalTrials.gov 2014. https://www.clinicaltrials.gov/ct2/show/NCT02178800?term=HPTN077&rank=1
Phase II safety and acceptability of an investigational injectable product, TMC278 LA, for pre-exposure prophylaxis (PrEP). ClinicalTrials.gov (2014). clinicaltrials.gov/ct2/show/NCT02165202?term=HPTN+076&rank=1
Kovarova M, Benhabbour SR, Massud I, Spagnuolo RA, Skinner B, Baker CE et al (2018) Ultra-long-acting removable drug delivery system for HIV treatment and prevention. Nat Commun 9(1):4156. https://doi.org/10.1038/s41467-018-06490-w
Partsch CJ, Sippell WG (2001) Pathogenesis and epidemiology of precocious puberty. Effects of exogenous oestrogens. Hum Reprod Update 7(3):292–302. https://doi.org/10.1093/humupd/7.3.292
Li P, Li Y, Yang CL (2014) Gonadotropin releasing hormone agonist treatment to increase final stature in children with precocious puberty: a meta-analysis. Medicine 93(27):e260. https://doi.org/10.1097/md.0000000000000260
Vercellini P, Buggio L, Berlanda N, Barbara G, Somigliana E, Bosari S (2016) Estrogen-progestins and progestins for the management of endometriosis. Fertil Steril 106(7):1552–71 e2. https://doi.org/10.1016/j.fertnstert.2016.10.022
Global report on diabetes (2016) World Health Organization. http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf. Accessed 22 Oct 2018
Donner T (2015) Insulin – pharmacology, therapeutic regimens and principles of intensive insulin therapy. [Updated 2015 Oct 12]. Endotext. South Dartmouth (MA): MDText.com, Inc
Mental health action plan 2013–2020 (2013) World Health Organization. http://www.who.int/iris/bitstream/10665/89966/1/9789241506021_eng.pdf?ua=1. Accessed 22 Oct 2018
Mental disorders Fact sheet (2018 Apr) World Health Organization. http://www.who.int/en/news-room/fact-sheets/detail/mental-disorders. Accessed 22 Oct 2018
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. https://doi.org/10.3322/caac.21492
Wolinsky JB, Colson YL, Grinstaff MW (2012) Local drug delivery strategies for cancer treatment: gels, nanoparticles, polymeric films, rods, and wafers. J Control Release 159(1):14–26. https://doi.org/10.1016/j.jconrel.2011.11.031
Carr DB, Cohen RI (2017) Are perioperative opioids obsolete? In: Proceedings of an IASP Acute Pain Special Interest Group Satellite Symposium September 25, 2016 Yokohama, Japan. PAIN Reports 2(4):e604. https://doi.org/10.1097/pr9.0000000000000604.
Werner MU, Kongsgaard UE (2014) I. Defining persistent post-surgical pain: is an update required? Br J Anaesth 113(1):1–4. https://doi.org/10.1093/bja/aeu012
Lavand’homme P, Pogatzki-Zahn E (2017) Fact sheet no. 4 chronic postsurgical pain: definition, impact, and prevention. International Association for the Study of Pain. http://www.iasp-pain.org/files/2017GlobalYear/FactSheets/4.%20Chronic%20Postsurgical%20Pain.LavandHomme-Zahn-EE_1485789834697_3.pdf. Accessed 22 Oct 2018
Shargel L, Andrew B, Wu-Pong S (2004) Chapter 17: modified-release drug products: introduction. In: Applied biopharmaceutics & pharmacokinetics, 5th edn. Appleton & Lange, Stamford
Oriowo MA, Landgren BM, Stenstrom B, Diczfalusy E (1980) A comparison of the pharmacokinetic properties of three estradiol esters. Contraception 21(4):415–424
Sanrame CN, Remenar JF, Blumberg LC, Waters J, Dean RL, Dong N et al (2014) Prodrugs of Pioglitazone for extended-release (XR) injectable formulations. Mol Pharm 11(10):3617–3623. https://doi.org/10.1021/mp500359a
Kostanski JW, Matsuda T, Nerurkar M, Naringrekar VH, inventors; Otsuka Pharmaceutical, assignee (2011) Controlled release sterile injectable aripiprazole formulation and method patent United States patent US8030313 B2
Francois MKJ, Dries WMAC, Basstanie EDG, inventors; Janssen Pharmaceutica, assignee (2003) Aqueous suspensions of submicron 9-hydroxyrisperidone fatty acid esters patent United States patent US6555544 B2
Blumberg LC, Zeidan TA, Maddaford A, Warren NC, Hutchison P (2013) Novel N-5-(acyloxyalkoxy)carbonyl prodrugs of olanzapine with physicochemical properties for extended-release. RSC Adv 3(37):16270–16278. https://doi.org/10.1039/C3RA41967C
Remenar JF (2014) Making the leap from daily oral dosing to long-acting injectables: lessons from the antipsychotics. Mol Pharm 11(6):1739–1749. https://doi.org/10.1021/mp500070m
Paquette SM, Dawit H, Hickey MB, Merisko-Liversidge E, Almarsson O, Deaver DR (2014) Long-acting atypical antipsychotics: characterization of the local tissue response. Pharm Res 31(8):2065–2077. https://doi.org/10.1007/s11095-014-1308-4
Angst MS, Drover DR (2006) Pharmacology of drugs formulated with DepoFoam™. Clin Pharmacokinet 45(12):1153–1176
Garcia LD, Zhu L, Lambert WJ, Patou G, inventors; Pacira Pharmaceuticals, Inc., assignee (2012) Sustained release formulation of a non-steroidal anti-inflammatory drug
Schutt EG, Mcguire RW, Walters PA, Los KD, inventors; Pacira Pharmaceuticals, Inc., assignee (2013) Method for formulating large diameter synthetic membrane vesicles
Spector MS, Zasadzinski JA, Sankaram MB (1996) Topology of multivesicular liposomes, a model biliquid foam. Langmuir 12(20):4704–4708. https://doi.org/10.1021/la960218s
Mantripragada S (2002) A lipid based depot (DepoFoam technology) for sustained release drug delivery. Prog Lipid Res 41(5):392–406
Willis RC, inventor DepoTech Corp, assignee (1999) Method for utilizing neutral lipids to modify in vivo release from multivesicular liposomes patent United States patent US 5,891,467, April 6
Sankaram M, Kim S, inventors; SkyePharma Inc, assignee (2000) Multivesicular liposomes with controlled release of encapsulated biologically active substances. Patent United States patent US 6,132,766, October 17
US Food and Drug Administration (2011) Chemistry review #2 NDA 22496 exparel (bupivacaine) liposomal injection US FDA. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/022496Orig1s000ChemR.pdf. Accessed 28 Oct 2018
Pacira Pharmaceuticals Inc (2008) Product label NDA 21–671/S-020 DEPODUR – morphine sulfate injection, lipid complex US Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021671s020lbl.pdf. Accessed 28 Oct 2018
Mont MA, Beaver WB, Dysart SH, Barrington JW, Del Gaizo DJ (2018) Local infiltration analgesia with liposomal bupivacaine improves pain scores and reduces opioid use after total knee arthroplasty: results of a randomized controlled trial. J Arthroplast 33(1):90–96. https://doi.org/10.1016/j.arth.2017.07.024
Gorfine SR, Onel E, Patou G, Krivokapic ZV (2011) Bupivacaine extended-release liposome injection for prolonged postsurgical analgesia in patients undergoing hemorrhoidectomy: a multicenter, randomized, double-blind, placebo-controlled trial. Dis Colon Rectum 54(12):1552–1559. https://doi.org/10.1097/DCR.0b013e318232d4c1
Lambrechts M, O’Brien MJ, Savoie FH, You Z (2013) Liposomal extended-release bupivacaine for postsurgical analgesia. Patient Prefer Adherence 7:885–890. https://doi.org/10.2147/PPA.S32175
Barrington JW, Emerson RH, Lovald ST, Lombardi AV, Berend KR (2017) No difference in early analgesia between liposomal bupivacaine injection and intrathecal morphine after TKA. Clin Orthop Relat Res 475(1):94–105. https://doi.org/10.1007/s11999-016-4931-z
Schwarzkopf R, Drexler M, Ma MW, Schultz VM, Le KT, Rutenberg TF et al (2016) Is there a benefit for liposomal bupivacaine compared to a traditional periarticular injection in total knee arthroplasty patients with a history of chronic opioid use? J Arthroplast 31(8):1702–1705. https://doi.org/10.1016/j.arth.2016.01.037
Dasta J, Ramamoorthy S, Patou G, Sinatra R (2012) Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin 28(10):1609–1615. https://doi.org/10.1185/03007995.2012.721760
Dorigo O, Oza AM, Tanyi JL, Strauss J, Pejovic T, Ghamande S et al (2018) 87PNew clinical data from the DeCidE1 trial: results on DPX-Survivac, low dose cyclophosphamide (CPA), and epacadostat (INCB024360) in subjects with advanced recurrent epithelial ovarian cancer. Ann Oncol 29(suppl_10.):mdy487.018-mdy487.018). https://doi.org/10.1093/annonc/mdy487.018
Langley JM, MacDonald LD, Weir GM, MacKinnon-Cameron D, Ye L, McNeil S et al (2018) A respiratory syncytial virus vaccine based on the small hydrophobic protein ectodomain presented with a novel lipid-based formulation is highly immunogenic and safe in adults: a first-in-humans study. J Infect Dis 218(3):378–387. https://doi.org/10.1093/infdis/jiy177
Brown RG, Pohajdak W, Kimmins WC, inventors; ImmunoVaccine Technologies Inc., assignee (2000) Vaccines with enhanced immune response and methods for their preparation patent United States patent US6793923B2
Brewer KD, Weir GM, Dude I, Davis C, Parsons C, Penwell A et al (2018) Unique depot formed by an oil based vaccine facilitates active antigen uptake and provides effective tumour control. J Biomed Sci 25(1):7. https://doi.org/10.1186/s12929-018-0413-9
Karkada M, Quinton T, Blackman R, Mansour M (2013) Tumor inhibition by DepoVax-based cancer vaccine is accompanied by reduced regulatory/suppressor cell proliferation and tumor infiltration. ISRN Oncol 2013:13. https://doi.org/10.1155/2013/753427
Mansour M, Sammatur L, MacDonald LD, Karkada M, Weir GM, Fuentes-Ortega A, inventors; ImmunoVaccine Technologies Inc., assignee (2008) Compositions comprising liposomes, an antigen, a polynucleotide and a carrier comprising a continuous phase of a hydrophobic substance patent United States patent US20110070298A1
Brewer KD, Lake K, Pelot N, Stanford MM, DeBay DR, Penwell A et al (2014) Clearance of depot vaccine SPIO-labeled antigen and substrate visualized using MRI. Vaccine 32(51):6956–6962. https://doi.org/10.1016/j.vaccine.2014.10.058
Laffont CM, Gomeni R, Zheng B, Heidbreder C, Fudala PJ, Nasser AF (2015) Population pharmacokinetic modeling and simulation to guide dose selection for RBP-7000, a new sustained-release formulation of risperidone. J Clin Pharmacol 55(1):93–103. https://doi.org/10.1002/jcph.366
Rademacher KH, Vahdat HL, Dorflinger L, Owen DH, Steiner MJ (2014) Global introduction of a low-cost contraceptive implant. In: Critical issues in reproductive health. Springer, Dordrecht, pp 285–306
Brache V (2014) WHO symposium WHO. Background and study methodology of a multicentre randomized clinical trial of two implantable contraceptives for women: jadelle and implanon. Eur J Contracept Reprod Health Care 19(1):S44
Bennink H (2000) The pharmacokinetics and pharmacodynamics of Implanon, a single-rod etonogestrel contraceptive implant. Eur J Contracept Reprod Health Care 5:12–20
Uhm S, Pope R, Schmidt A, Bazella C, Perriera L (2016) Home or office etonogestrel implant insertion after pregnancy: a randomized trial. Contraception 94(5):567–571
Wong I, Teoh S, Yeoh A, Lingam G (2013) Sustained-release ganciclovir implant as prophylaxis for cytomegalovirus retinitis in a child undergoing bone marrow transplantation. Eye 27(7):890
Schlegel P (2009) A review of the pharmacokinetic and pharmacological properties of a once-yearly administered histrelin acetate implant in the treatment of prostate cancer. BJU Int 103:7–13
Shi Y, Li L (2005) Current advances in sustained-release systems for parenteral drug delivery. Expert Opin Drug Deliv 2(6):1039–1058
Aoki T, Nishikawa R, Sugiyama K, Nonoguchi N, Kawabata N, Mishima K et al (2014) A multicenter phase I/II study of the BCNU implant (Gliadel® wafer) for Japanese patients with malignant gliomas. Neurol Med Chir 54(4):290–301
Inc. S-aC (2015) Product monograph, PrSUPREFACT® Buserelin Acetate. 2905 Place Louis-R.-Renaud, Laval (Québec) H7V 0A3. http://products.sanofi.ca/en/suprefact.pdf. Accessed 05 Jan 2019
Henry RR, Rosenstock J, Logan D, Alessi T, Luskey K, Baron MA (2014) Continuous subcutaneous delivery of exenatide via ITCA 650 leads to sustained glycemic control and weight loss for 48 weeks in metformin-treated subjects with type 2 diabetes. J Diabetes Complicat 28(3):393–398
Yue B, Brendel R, Lukitsch A, Prentice T, Doty B (2017) Solubility and stability of baclofen 3 mg/mL intrathecal formulation and its compatibility with implantable programmable intrathecal infusion systems. Neuromodulation 20(4):397–404
Kumar A, Pillai J (2018) Implantable drug delivery systems: an overview. In: Nanostructures for the engineering of cells, tissues and organs. Elsevier, Oxford, pp 473–511
Nunes-Pereira J, Ribeiro S, Ribeiro C, Gombek CJ, Gama F, Gomes A et al (2015) Poly (vinylidene fluoride) and copolymers as porous membranes for tissue engineering applications. Polym Test 44:234–241
Tian W, Mahmoudi M, Lhermusier T, Kiramijyan S, Chen F, Torguson R et al (2016) The influence of advancing age on implantation of drug-eluting stents. Catheter Cardiovasc Interv 88(4):516–521
Dunn RL, English JP, Cowsar DR, Vanderbilt DP, inventors; Atrix Laboratories Inc assignee (1988–1994) Biodegradable in-situ forming implants and methods of producing the same patent US Patent nos. US4938763B1, US07513782, US07788032, US07788159, US08210891
Chen S, Pieper R, Webster DC, Singh J (2005) Triblock copolymers: synthesis, characterization, and delivery of a model protein. Int J Pharm 288(2):207–218
Loh XJ, Goh SH, Li J (2007) New biodegradable thermogelling copolymers having very low gelation concentrations. Biomacromolecules 8(2):585–593. https://doi.org/10.1021/bm0607933
Liu CB, Gong CY, Huang MJ, Wang JW, Pan YF, Zhang YD et al (2008) Thermoreversible gel–sol behavior of biodegradable PCL-PEG-PCL triblock copolymer in aqueous solutions. J Biomed Mater Res B Appl Biomater 84B(1):165–175. https://doi.org/10.1002/jbm.b.30858
Zhai Y, Deng L, Xing J, Liu Y, Zhang Q, Dong A (2009) A new injectable thermogelling material: methoxy poly(ethylene glycol)–poly(sebacic acid-D,L-lactic acid)–methoxy poly(ethylene glycol) triblock co-polymer. J Biomater Sci Polym Ed 20(7–8):923–934. https://doi.org/10.1163/156856209X444349
Petit A, Redout EM, van de Lest CH, de Grauw JC, Müller B, Meyboom R et al (2015) Sustained intra-articular release of celecoxib from in situ forming gels made of acetyl-capped PCLA-PEG-PCLA triblock copolymers in horses. Biomaterials 53:426–436. https://doi.org/10.1016/j.biomaterials.2015.02.109
Zentner GM, Rathi R, Shih C, McRea JC, Seo M-H, Oh H et al (2001) Biodegradable block copolymers for delivery of proteins and water-insoluble drugs. J Control Release 72(1):203–215. https://doi.org/10.1016/S0168-3659(01)00276-0
Elstad NL, Fowers KD (2009) OncoGel (ReGel/paclitaxel) – clinical applications for a novel paclitaxel delivery system. Adv Drug Deliv Rev 61(10):785–794. https://doi.org/10.1016/j.addr.2009.04.010
DeWitt JM, Murthy SK, Ardhanari R, DuVall GA, Wallner G, Litka P et al (2017) EUS-guided paclitaxel injection as an adjunctive therapy to systemic chemotherapy and concurrent external beam radiation before surgery for localized or locoregional esophageal cancer: a multicenter prospective randomized trial. Gastrointest Endosc 86(1):140–149. https://doi.org/10.1016/j.gie.2016.11.017
DuVall GA, Tarabar D, Seidel RH, Elstad NL, Fowers KD (2009) Phase 2: a dose-escalation study of OncoGel (ReGel/paclitaxel), a controlled-release formulation of paclitaxel, as adjunctive local therapy to external-beam radiation in patients with inoperable esophageal cancer. Anti-Cancer Drugs 20(2):89–95. https://doi.org/10.1097/CAD.0b013e3283222c12
Vukelja SJ, Anthony SP, Arseneau JC, Berman BS, Cunningham CC, Nemunaitis JJ et al (2007) Phase 1 study of escalating-dose OncoGel (ReGel/paclitaxel) depot injection, a controlled-release formulation of paclitaxel, for local management of superficial solid tumor lesions. Anti-Cancer Drugs 18(3):283–289. https://doi.org/10.1097/CAD.0b013e328011a51d
Tellegen AR, Willems N, Beukers M, Grinwis GCM, Plomp SGM, Bos C et al (2018) Intradiscal application of a PCLA–PEG–PCLA hydrogel loaded with celecoxib for the treatment of back pain in canines: what’s in it for humans? J Tissue Eng Regen Med 12(3):642–652. https://doi.org/10.1002/term.2483
Durect Corporation (2017) DURECT announces top-line results from the PERSIST phase 3 trial of POSIMIR® (SABER®-Bupivacaine) did not meet primary efficacy endpoint. PR Newswire
Pavel M, Borson-Chazot F, Cailleux A, Horsch D, Lahner H, Pivonello R et al (2018) Octreotide SC depot in patients with acromegaly and functioning neuroendocrine tumors: a phase 2, multicenter study. Cancer Chemother Pharmacol. https://doi.org/10.1007/s00280-018-3734-1
Bhattarai N, Gunn J, Zhang M (2010) Chitosan-based hydrogels for controlled, localized drug delivery. Adv Drug Deliv Rev 62(1):83–99
Ruel-Gariépy E, Shive M, Bichara A, Berrada M, Le Garrec D, Chenite A et al (2004) A thermosensitive chitosan-based hydrogel for the local delivery of paclitaxel. Eur J Pharm Biopharm 57(1):53–63
Park KM, Lee SY, Joung YK, Na JS, Lee MC, Park KD (2009) Thermosensitive chitosan–pluronic hydrogel as an injectable cell delivery carrier for cartilage regeneration. Acta Biomater 5(6):1956–1965
Kim K, Park S, Yang J-A, Jeon J-H, Bhang S, Kim B-S et al (2011) Injectable hyaluronic acid–tyramine hydrogels for the treatment of rheumatoid arthritis. Acta Biomater 7(2):666–674
Kim J, Kim IS, Cho TH, Lee KB, Hwang SJ, Tae G et al (2007) Bone regeneration using hyaluronic acid-based hydrogel with bone morphogenic protein-2 and human mesenchymal stem cells. Biomaterials 28(10):1830–1837
George M, Abraham TE (2006) Polyionic hydrocolloids for the intestinal delivery of protein drugs: alginate and chitosan—a review. J Control Release 114(1):1–14
LeRoux MA, Guilak F, Setton LA (1999) Compressive and shear properties of alginate gel: effects of sodium ions and alginate concentration. J Biomed Mater Res 47(1):46–53
Freeman I, Kedem A, Cohen S (2008) The effect of sulfation of alginate hydrogels on the specific binding and controlled release of heparin-binding proteins. Biomaterials 29(22):3260–3268
Lee K, Lee H, Bae KH, Park TG (2010) Heparin immobilized gold nanoparticles for targeted detection and apoptotic death of metastatic cancer cells. Biomaterials 31(25):6530–6536
Michalopoulos GK, DeFrances MC (1997) Liver regeneration. Science 276(5309):60–66
Ibusuki S, Fujii Y, Iwamoto Y, Matsuda T (2003) Tissue-engineered cartilage using an injectable and in situ gelable thermoresponsive gelatin: fabrication and in vitro performance. Tissue Eng 9(2):371–384
Davis H, Miller S, Case E, Leach J (2011) Supplementation of fibrin gels with sodium chloride enhances physical properties and ensuing osteogenic response. Acta Biomater 7(2):691–699
Jin R, Teixeira LM, Dijkstra PJ, Karperien M, Van Blitterswijk C, Zhong Z et al (2009) Injectable chitosan-based hydrogels for cartilage tissue engineering. Biomaterials 30(13):2544–2551
Kobayashi S, Uyama H, Kimura S (2001) Enzymatic polymerization. Chem Rev 101(12):3793–3818
Tran NQ, Joung YK, Lih E, Park KD (2011) In situ forming and rutin-releasing chitosan hydrogels as injectable dressings for dermal wound healing. Biomacromolecules 12(8):2872–2880
Tran NQ, Joung YK, Lih E, Park KM, Park KD (2010) Supramolecular hydrogels exhibiting fast in situ gel forming and adjustable degradation properties. Biomacromolecules 11(3):617–625
Ding C, Zhao L, Liu F, Cheng J, Gu J, Dan S- et al. Dually responsive injectable hydrogel prepared by in situ cross-linking of glycol chitosan and benzaldehyde-capped PEO-PPO-PEO. Biomacromolecules 2010;11(4):1043–1051.
Kim MS, Choi YJ, Noh I, Tae G (2007) Synthesis and characterization of in situ chitosan-based hydrogel via grafting of carboxyethyl acrylate. J Biomed Mater Res A 83(3):674–682
Sakloetsakun D, Hombach JM, Bernkop-Schnürch A (2009) In situ gelling properties of chitosan-thioglycolic acid conjugate in the presence of oxidizing agents. Biomaterials 30(31):6151–6157
Tan H, Chu CR, Payne KA, Marra KG (2009) Injectable in situ forming biodegradable chitosan–hyaluronic acid based hydrogels for cartilage tissue engineering. Biomaterials 30(13):2499–2506
D-y T, Z-m W, X-g Z, Y-x W, Zheng C, Wang Z et al (2010) Synthesis and characterization of in situ cross-linked hydrogel based on self-assembly of thiol-modified chitosan with PEG diacrylate using Michael type addition. Polymer 51(3):639–646
Zhang H, Qadeer A, Mynarcik D, Chen W (2011) Delivery of rosiglitazone from an injectable triple interpenetrating network hydrogel composed of naturally derived materials. Biomaterials 32(3):890–898
Freiberg S, Zhu X (2004) Polymer microspheres for controlled drug release. Int J Pharm 282(1–2):1–18
Wright SG, Christenson T, Yeah TY, Rickey ME, Hotz JM, Kumar R et al., inventors; Alkermes Inc., assignee (2004) Polymer-based sustained release device patent US Patent US7456254B2
Wright SG, Rickey ME, Ramstack JM, Lyons SL, Hotz JM, inventors; Alkermes Inc., assignee (2000) Method for preparing microparticles having a selected polymer molecular weight patent US Patent US6264987B1
Dormer N, Berkland C, inventors; Orbis Biosciences, Inc., assignee. Biodegradable polymer microsphere compositions for parenteral administration patent WO application WO2017189645A1. 2016.
Berkland C, Kim K, Pack DW (2001) Fabrication of PLG microspheres with precisely controlled and monodisperse size distributions. J Control Release 73(1):59–74. https://doi.org/10.1016/S0168-3659(01)00289-9
Berkland C, King M, Cox A, Kim KK, Pack DW (2002) Precise control of PLG microsphere size provides enhanced control of drug release rate. J Control Release 82(1):137–147
Berkland C, Pollauf E, Varde N, Pack DW, Kim K (2007) Monodisperse liquid-filled biodegradable microcapsules. Pharm Res 24(5):1007–1013. https://doi.org/10.1007/s11095-006-9197-9
Lew B, Kim IY, Choi H, Kim KK (2018) Sustained exenatide delivery via intracapsular microspheres for improved survival and function of microencapsulated porcine islets. Drug Deliv Transl Res 8(3):857–862. https://doi.org/10.1007/s13346-018-0484-x
Plexis TM (2016) http://www.auritecpharma.com/plexis/
Smith T, inventor Auritec Pharmaceuticals, assignee. Coated particles for sustained-release pharmaceutical administration patent US Patent US9492388B2. 2002.
Schneider EL, Henise J, Reid R, Ashley GW, Santi DV (2016) Subcutaneously administered self-cleaving hydrogel–octreotide conjugates provide very long-acting octreotide. Bioconjug Chem 27(7):1638–1644. https://doi.org/10.1021/acs.bioconjchem.6b00188
Schneider EL, Hearn BR, Pfaff SJ, Reid R, Parkes DG, Vrang N et al (2017) A hydrogel-microsphere drug delivery system that supports once-monthly administration of a GLP-1 receptor agonist. ACS Chem Biol 12(8):2107–2116
Vhora I, Patil S, Bhatt P, Gandhi R, Baradia D, Misra A (2014) Receptor-targeted drug delivery: current perspective and challenges. Ther Deliv 5(9):1007–1024. https://doi.org/10.4155/tde.14.63
Bhatt P, Vhora I, Patil S, Amrutiya J, Bhattacharya C, Misra A et al (2016) Role of antibodies in diagnosis and treatment of ovarian cancer: basic approach and clinical status. J Control Release 226:148–167. https://doi.org/10.1016/j.jconrel.2016.02.008
Vhora I, Patil S, Bhatt P, Misra A (2015) Chapter one – protein– and peptide–drug conjugates: an emerging drug delivery technology. In: Donev R (ed) Advances in protein chemistry and structural biology. Academic, Waltham, pp 1–55
Bawa P, Pillay V, Choonara YE, Du Toit LC (2009) Stimuli-responsive polymers and their applications in drug delivery. Biomed Mater 4(2):022001
Bae YH, Park K (2011) Targeted drug delivery to tumors: myths, reality and possibility. J Control Release 153(3):198
Hosseini M, Farjadian F, Makhlouf ASH (2016) Smart stimuli-responsive nano-sized hosts for drug delivery. In: Industrial applications for intelligent polymers and coatings. Springer, Cham, pp 1–26
Rhee Y-S, Park C-W, DeLuca PP, Mansour HM. Sustained-release injectable drug delivery. 2010.
Gulati N, Gupta H (2011) Parenteral drug delivery: a review. Recent Pat Drug Deliv Formulation 5(2):133–145
Ganta S, Devalapally H, Shahiwala A, Amiji M (2008) A review of stimuli-responsive nanocarriers for drug and gene delivery. J Control Release 126(3):187–204
Gupta P, Vermani K, Garg S (2002) Hydrogels: from controlled release to pH-responsive drug delivery. Drug Discov Today 7(10):569–579
Kost J, Langer R (2012) Responsive polymeric delivery systems. Adv Drug Deliv Rev 64:327–341
Bae Y, Fukushima S, Harada A, Kataoka K (2003) Design of environment-sensitive supramolecular assemblies for intracellular drug delivery: polymeric micelles that are responsive to intracellular pH change. Angew Chem 115(38):4788–4791
Qiu Y, Park K (2001) Environment-sensitive hydrogels for drug delivery. Adv Drug Deliv Rev 53(3):321–339
Gisbert-Garzarán M, Manzano M, Vallet-Regí M (2017) pH-responsive mesoporous silica and carbon nanoparticles for drug delivery. Bioengineering 4(1):3
Sawant RM, Hurley J, Salmaso S, Kale A, Tolcheva E, Levchenko T et al (2006) “SMART” drug delivery systems: double-targeted pH-responsive pharmaceutical nanocarriers. Bioconjug Chem 17(4):943–949
Yang W-W, Pierstorff E (2012) Reservoir-based polymer drug delivery systems. J Lab Autom 17(1):50–58
Yoshida T, Lai TC, Kwon GS, Sako K (2013) pH-and ion-sensitive polymers for drug delivery. Expert Opin Drug Deliv 10(11):1497–1513
Zhou L, Liang D, He X, Li J, Tan H, Li J et al (2012) The degradation and biocompatibility of pH-sensitive biodegradable polyurethanes for intracellular multifunctional antitumor drug delivery. Biomaterials 33(9):2734–2745
Kratz F (2007) DOXO-EMCH (INNO-206): the first albumin-binding prodrug of doxorubicin to enter clinical trials. Expert Opin Investig Drugs 16(6):855–866
Zhao L, Zhu L, Liu F, Liu C, Wang Q, Zhang C et al (2011) pH triggered injectable amphiphilic hydrogel containing doxorubicin and paclitaxel. Int J Pharm 410(1–2):83–91
Knorr V, Russ V, Allmendinger L, Ogris M, Wagner E (2008) Acetal linked oligoethylenimines for use as pH-sensitive gene carriers. Bioconjug Chem 19(8):1625–1634
Tu C, Zhu L, Qiu F, Wang D, Su Y, Zhu X et al (2013) Facile PEGylation of Boltorn® H40 for pH-responsive drug carriers. Polymer 54(8):2020–2027
Garbern JC, Minami E, Stayton PS, Murry CE (2011) Delivery of basic fibroblast growth factor with a pH-responsive, injectable hydrogel to improve angiogenesis in infarcted myocardium. Biomaterials 32(9):2407–2416
Thambi T, Deepagan V, Yoo CK, Park JH (2011) Synthesis and physicochemical characterization of amphiphilic block copolymers bearing acid-sensitive orthoester linkage as the drug carrier. Polymer 52(21):4753–4759
Sánchez M, Aranda FJ, Teruel JA, Ortiz A (2011) New pH-sensitive liposomes containing phosphatidylethanolamine and a bacterial dirhamnolipid. Chem Phys Lipids 164(1):16–23
Vhora I, Lalani R, Bhatt P, Patil S, Misra A (2019) Lipid-nucleic acid nanoparticles of novel ionizable lipids for systemic BMP-9 gene delivery to bone-marrow mesenchymal stem cells for osteoinduction. Int J Pharm 563:324–336
Midoux P, Pichon C, Yaouanc J-J, Jaffrès P-A (2009) Chemical vectors for gene delivery: a current review on polymers, peptides and lipids containing histidine or imidazole as nucleic acids carriers. Br J Pharmacol 157(2):166–178. https://doi.org/10.1111/j.1476-5381.2009.00288.x
Yuba E, Kojima C, Harada A, Watarai S, Kono K (2010) pH-Sensitive fusogenic polymer-modified liposomes as a carrier of antigenic proteins for activation of cellular immunity. Biomaterials 31(5):943–951
Yatvin M, Kreutz W, Horwitz B, Shinitzky M (1980) pH-sensitive liposomes: possible clinical implications. Science 210(4475):1253–1255
Cazzola R, Viani P, Allevi P, Cighetti G, Cestaro B (1997) pH sensitivity and plasma stability of liposomes containing N-stearoylcysteamine. Biochimica et Biophysica Acta (BBA)-Biomembranes 1329(2):291–301
Parente R, Nir S, Szoka F (1988) pH-dependent fusion of phosphatidylcholine small vesicles. Induction by a synthetic amphipathic peptide. J Biol Chem 263(10):4724–4730
Tycko B, Maxfield FR (1982) Rapid acidification of endocytic vesicles containing α2-macroglobulin. Cell 28(3):643–651
Kim D, Lee ES, Oh KT, Gao ZG, Bae YH (2008) Doxorubicin-loaded polymeric micelle overcomes multidrug resistance of cancer by double-targeting folate receptor and early endosomal pH. Small 4(11):2043–2050
Alberts B, Bray D, Lewis J, Raff M, Roberts K, Watson J (1994) Molecular biology of the cell. Garland, New York. Google Scholar. 907–82
Renoux B, Raes F, Legigan T, Péraudeau E, Eddhif B, Poinot P et al (2017) Targeting the tumour microenvironment with an enzyme-responsive drug delivery system for the efficient therapy of breast and pancreatic cancers. Chem Sci 8(5):3427–3433
Tukappa A, Ultimo A, de la Torre C, Pardo T, Sancenón F, Martínez-Máñez R (2016) Polyglutamic acid-gated mesoporous silica nanoparticles for enzyme-controlled drug delivery. Langmuir 32(33):8507–8515
Itoh Y, Matsusaki M, Kida T, Akashi M (2006) Enzyme-responsive release of encapsulated proteins from biodegradable hollow capsules. Biomacromolecules 7(10):2715–2718
Yao Q, Kou L, Tu Y, Zhu L (2018) Mmp-responsive ‘smart’drug delivery and tumor targeting. Trends Pharmacol Sci 39(8):766–781
Böttger R, Knappe D, Hoffmann R (2016) Readily adaptable release kinetics of prodrugs using protease-dependent reversible PEGylation. J Control Release 230:88–94
Zhu L, Kate P, Torchilin VP (2012) Matrix metalloprotease 2-responsive multifunctional liposomal nanocarrier for enhanced tumor targeting. ACS Nano 6(4):3491–3498
Zhang C, Pan D, Luo K, She W, Guo C, Yang Y et al (2014) Peptide dendrimer–doxorubicin conjugate-based nanoparticles as an enzyme-responsive drug delivery system for cancer therapy. Adv Healthcare Mater 3(8):1299–1308
Singer JW, Shaffer S, Baker B, Bernareggi A, Stromatt S, Nienstedt D et al (2005) Paclitaxel poliglumex (XYOTAX; CT-2103): an intracellularly targeted taxane. Anti-Cancer Drugs 16(3):243–254
Shaffer SA, Baker-Lee C, Kennedy J, Lai MS, de Vries P, Buhler K et al (2007) In vitro and in vivo metabolism of paclitaxel poliglumex: identification of metabolites and active proteases. Cancer Chemother Pharmacol 59(4):537–548
Melancon MP, Li C (2011) Multifunctional synthetic poly (L-glutamic Acid)–based cancer therapeutic and imaging agents. Mol Imaging 10(1):7290.2011. 00007
Scott KF, Sajinovic M, Hein J, Nixdorf S, Galettis P, Liauw W et al (2010) Emerging roles for phospholipase A2 enzymes in cancer. Biochimie 92(6):601–610
Schafer FQ, Buettner GR (2001) Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free Radic Biol Med 30(11):1191–1212
Meng F, Cheng R, Deng C, Zhong Z (2012) Intracellular drug release nanosystems. Mater Today 15(10):436–442
Li Y, Lokitz BS, Armes SP, McCormick CL (2006) Synthesis of reversible shell cross-linked micelles for controlled release of bioactive agents. Macromolecules 39(8):2726–2728
Vachutinsky Y, Oba M, Miyata K, Hiki S, Kano MR, Nishiyama N et al (2011) Antiangiogenic gene therapy of experimental pancreatic tumor by sFlt-1 plasmid DNA carried by RGD-modified crosslinked polyplex micelles. J Control Release 149(1):51–57
Zhang L, Liu W, Lin L, Chen D, Stenzel MH (2008) Degradable disulfide core-cross-linked micelles as a drug delivery system prepared from vinyl functionalized nucleosides via the RAFT process. Biomacromolecules 9(11):3321–3331
Wu J, Zhao L, Xu X, Bertrand N, Choi WI, Yameen B et al (2015) Hydrophobic Cysteine Poly (disulfide)-based Redox-hypersensitive nanoparticle platform for cancer theranostics. Angew Chem Int Ed 54(32):9218–9223
Manickam DS, Li J, Putt DA, Zhou Q-H, Wu C, Lash LH et al (2010) Effect of innate glutathione levels on activity of redox-responsive gene delivery vectors. J Control Release 141(1):77–84
Zhong P, Zhang J, Deng C, Cheng R, Meng F, Zhong Z (2016) Glutathione-sensitive hyaluronic acid-SS-mertansine prodrug with a high drug content: facile synthesis and targeted breast tumor therapy. Biomacromolecules 17(11):3602–3608
Wen H, Li Y (2014) Redox sensitive nanoparticles with disulfide bond linked sheddable shell for intracellular drug delivery. Med Chem 4(11):748–755
Zhai S, Hu X, Hu Y, Wu B, Xing D (2017) Visible light-induced crosslinking and physiological stabilization of diselenide-rich nanoparticles for redox-responsive drug release and combination chemotherapy. Biomaterials 121:41–54
Huo M, Yuan J, Tao L, Wei Y (2014) Redox-responsive polymers for drug delivery: from molecular design to applications. Polym Chem 5(5):1519–1528
Baldwin AD, Kiick KL (2013) Reversible maleimide–thiol adducts yield glutathione-sensitive poly (ethylene glycol)–heparin hydrogels. Polym Chem 4(1):133–143
Wu Q, Wang L, Yu H, Wang J, Chen Z (2011) Organization of glucose-responsive systems and their properties. Chem Rev 111(12):7855–7875
Webber MJ, Anderson DG (2015) Smart approaches to glucose-responsive drug delivery. J Drug Target 23(7–8):651–655
Ravaine V, Ancla C, Catargi B (2008) Chemically controlled closed-loop insulin delivery. J Control Release 132(1):2–11
Takemoto Y, Ajiro H, T-a A, Akashi M (2010) Fabrication of surface-modified hydrogels with polyion complex for controlled release. Chem Mater 22(9):2923–2929
Sun C, Lee JS, Zhang M (2008) Magnetic nanoparticles in MR imaging and drug delivery. Adv Drug Deliv Rev 60(11):1252–1265
Karimi M, Ghasemi A, Zangabad PS, Rahighi R, Basri SMM, Mirshekari H et al (2016) Smart micro/nanoparticles in stimulus-responsive drug/gene delivery systems. Chem Soc Rev 45(5):1457–1501
Hayashi K, Ono K, Suzuki H, Sawada M, Moriya M, Sakamoto W et al (2010) High-frequency, magnetic-field-responsive drug release from magnetic nanoparticle/organic hybrid based on hyperthermic effect. ACS Appl Mater Interfaces 2(7):1903–1911
Jeon H, Kim J, Lee YM, Kim J, Choi HW, Lee J et al (2016) Poly-paclitaxel/cyclodextrin-SPION nano-assembly for magnetically guided drug delivery system. J Control Release 231:68–76
Wahajuddin SA (2012) Superparamagnetic iron oxide nanoparticles: magnetic nanoplatforms as drug carriers. Int J Nanomedicine 7:3445
Jenkins SI, Weinberg D, Al-Shakli AF, Fernandes AR, Yiu HH, Telling ND et al (2016) ‘Stealth’nanoparticles evade neural immune cells but also evade major brain cell populations: implications for PEG-based neurotherapeutics. J Control Release 224:136–145
Xiong F, Chen Y, Chen J, Yang B, Zhang Y, Gao H et al (2013) Rubik-like magnetic nanoassemblies as an efficient drug multifunctional carrier for cancer theranostics. J Control Release 172(3):993–1001
Liu D, Wu W, Chen X, Wen S, Zhang X, Ding Q et al (2012) Conjugation of paclitaxel to iron oxide nanoparticles for tumor imaging and therapy. Nanoscale 4(7):2306–2310
Johnson J (2002) Magnetics business & technology magazine – premier issue. http://www.magneticsmagazine.com/eprints/FeRx.htm
Creixell M, Bohorquez AC, Torres-Lugo M, Rinaldi C (2011) EGFR-targeted magnetic nanoparticle heaters kill cancer cells without a perceptible temperature rise. ACS Nano 5(9):7124–7129
Gordon R, Hines J, Gordon D (1979) Intracellular hyperthermia a biophysical approach to cancer treatment via intracellular temperature and biophysical alterations. Med Hypotheses 5(1):83–102
Dutz S, Hergt R (2013) Magnetic nanoparticle heating and heat transfer on a microscale: basic principles, realities and physical limitations of hyperthermia for tumour therapy. Int J Hyperth 29(8):790–800
Ortega D, Pankhurst QA (2013) Magnetic hyperthermia. Nanoscience 1(60):e88
Torchilin VP (2014) Multifunctional, stimuli-sensitive nanoparticulate systems for drug delivery. Nat Rev Drug Discov 13(11):813
Chilkoti A, Dreher MR, Meyer DE, Raucher D (2002) Targeted drug delivery by thermally responsive polymers. Adv Drug Deliv Rev 54(5):613–630
Arouri A, Mouritsen OG (2013) Membrane-perturbing effect of fatty acids and lysolipids. Prog Lipid Res 52(1):130–140
Mills JK, Needham D (2005) Lysolipid incorporation in dipalmitoylphosphatidylcholine bilayer membranes enhances the ion permeability and drug release rates at the membrane phase transition. Biochimica et Biophysica Acta (BBA)-Biomembranes 1716(2):77–96
Kong G, Anyarambhatla G, Petros WP, Braun RD, Colvin OM, Needham D et al (2000) Efficacy of liposomes and hyperthermia in a human tumor xenograft model: importance of triggered drug release. Cancer Res 60(24):6950–6957
De Smet M, Langereis S, van den Bosch S, Grüll H (2010) Temperature-sensitive liposomes for doxorubicin delivery under MRI guidance. J Control Release 143(1):120–127
Loo C, Lin A, Hirsch L, Lee M-H, Barton J, Halas N et al (2004) Nanoshell-enabled photonics-based imaging and therapy of cancer. Technol Cancer Res Treat 3(1):33–40
Oldenburg S, Averitt R, Westcott S, Halas N (1998) Nanoengineering of optical resonances. Chem Phys Lett 288(2–4):243–247
Hirsch LR, Stafford RJ, Bankson J, Sershen SR, Rivera B, Price R et al (2003) Nanoshell-mediated near-infrared thermal therapy of tumors under magnetic resonance guidance. Proc Natl Acad Sci 100(23):13549–13554
Tagami T, Ernsting MJ, Li S-D (2011) Efficient tumor regression by a single and low dose treatment with a novel and enhanced formulation of thermosensitive liposomal doxorubicin. J Control Release 152(2):303–309
Korenaga K, Korenaga M, Hino K, Sakaida I (2009) Usefulness of sonazoid-contrast enhanced ultrasonography for hepatocellular carcinoma: comparison with pathological diagnosis and superparamagnetic iron oxide magnetic resonance images: 931. Hepatology 50:743A
Cheng Y, Hao J, Lee LA, Biewer MC, Wang Q, Stefan MC (2012) Thermally controlled release of anticancer drug from self-assembled γ-substituted amphiphilic poly (ε-caprolactone) micellar nanoparticles. Biomacromolecules 13(7):2163–2173
Paris JL, Cabañas MV, Manzano M, Vallet-Regí M (2015) Polymer-grafted mesoporous silica nanoparticles as ultrasound-responsive drug carriers. ACS Nano 9(11):11023–11033
Marin A, Muniruzzaman M, Rapoport N (2001) Acoustic activation of drug delivery from polymeric micelles: effect of pulsed ultrasound. J Control Release 71(3):239–249
Rapoport N (2012) Ultrasound-mediated micellar drug delivery. Int J Hyperth 28(4):374–385
Watanabe R, Matsumura M, Munemasa T, Fujimaki M, Suematsu M (2007) Mechanism of hepatic parenchyma-specific contrast of microbubble-based contrast agent for ultrasonography: microscopic studies in rat liver. Investig Radiol 42(9):643–651
Suzuki R, Oda Y, Omata D, Nishiie N, Koshima R, Shiono Y et al (2016) Tumor growth suppression by the combination of nanobubbles and ultrasound. Cancer Sci 107(3):217–223
Lentacker I, Geers B, Demeester J, De Smedt SC, Sanders NN (2010) Design and evaluation of doxorubicin-containing microbubbles for ultrasound-triggered doxorubicin delivery: cytotoxicity and mechanisms involved. Mol Ther 18(1):101–108
Deng Z, Yan F, Jin Q, Li F, Wu J, Liu X et al (2014) Reversal of multidrug resistance phenotype in human breast cancer cells using doxorubicin-liposome–microbubble complexes assisted by ultrasound. J Control Release 174:109–116
Myhr G, Moan J (2006) Synergistic and tumour selective effects of chemotherapy and ultrasound treatment. Cancer Lett 232(2):206–213
Shum P, Kim J-M, Thompson DH (2001) Phototriggering of liposomal drug delivery systems. Adv Drug Deliv Rev 53(3):273–284
Fomina N, Sankaranarayanan J, Almutairi A (2012) Photochemical mechanisms of light-triggered release from nanocarriers. Adv Drug Deliv Rev 64(11):1005–1020
Alvarez-Lorenzo C, Bromberg L, Concheiro A (2009) Light-sensitive intelligent drug delivery systems. Photochem Photobiol 85(4):848–860
Linsley CS, Wu BM (2017) Recent advances in light-responsive on-demand drug-delivery systems. Ther Deliv 8(2):89–107
Normand N, Valamanesh F, Savoldelli M, Mascarelli F, BenEzra D, Courtois Y et al (2005) VP22 light controlled delivery of oligonucleotides to ocular cells in vitro and in vivo. Mol Vis 11(21):184–191
Schmidt-Erfurth U, Hasan T (2000) Mechanisms of action of photodynamic therapy with verteporfin for the treatment of age-related macular degeneration. Surv Ophthalmol 45(3):195–214
Vhora I, Patil S, Amrutiya J, Misra A (2015) Liposomes and lipid envelope-type systems for systemic siRNA delivery. Curr Pharm Des 21(31):4541–4555
Khatri N, Baradia D, Vhora I, Rathi M, Misra A (2014) cRGD grafted liposomes containing inorganic nano-precipitate complexed siRNA for intracellular delivery in cancer cells. J Control Release 182:45–57. https://doi.org/10.1016/j.jconrel.2014.03.003
Vhora I, Lalani R, Bhatt P, Patil S, Patel H, Patel V et al (2018) Colloidally stable small unilamellar stearyl amine lipoplexes for effective BMP-9 gene delivery to stem cells for osteogenic differentiation. AAPS PharmSciTech. https://doi.org/10.1208/s12249-018-1161-6
Khatri N, Baradia D, Vhora I, Rathi M, Misra A (2014) Development and characterization of siRNA lipoplexes: effect of different lipids, in vitro evaluation in cancerous cell lines and in vivo toxicity study. AAPS PharmSciTech 15(6):1630–1643. https://doi.org/10.1208/s12249-014-0193-9
Patil S, Lalani R, Bhatt P, Vhora I, Patel V, Patel H et al (2018) Hydroxyethyl substituted linear polyethylenimine for safe and efficient delivery of siRNA therapeutics. RSC Adv 8(62):35461–35473. https://doi.org/10.1039/C8RA06298F
Bhatt P, Khatri N, Kumar M, Baradia D, Misra A (2015) Microbeads mediated oral plasmid DNA delivery using polymethacrylate vectors: an effectual groundwork for colorectal cancer. Drug Delivery 22(6):849–861. https://doi.org/10.3109/10717544.2014.898348
Patil S, Bhatt P, Lalani R, Amrutiya J, Vhora I, Kolte A et al (2016) Low molecular weight chitosan–protamine conjugate for siRNA delivery with enhanced stability and transfection efficiency. RSC Adv 6(112):110951–110963
Vhora I, Khatri N, Desai J, Thakkar HP (2014) Caprylate-conjugated cisplatin for the development of novel liposomal formulation. AAPS PharmSciTech 15(4):845–857. https://doi.org/10.1208/s12249-014-0106-y
Bhatt P, Lalani R, Vhora I, Patil S, Amrutiya J, Misra A et al (2018) Liposomes encapsulating native and cyclodextrin enclosed paclitaxel: enhanced loading efficiency and its pharmacokinetic evaluation. Int J Pharm 536(1):95–107. https://doi.org/10.1016/j.ijpharm.2017.11.048
Allmendinger A, Fischer S, Huwyler J, Mahler H-C, Schwarb E, Zarraga IE et al (2014) Rheological characterization and injection forces of concentrated protein formulations: an alternative predictive model for non-Newtonian solutions. Eur J Pharm Biopharm 87(2):318–328. https://doi.org/10.1016/j.ejpb.2014.01.009
Liu J, Nguyen MDH, Andya JD, Shire SJ (2005) Reversible self-association increases the viscosity of a concentrated monoclonal antibody in aqueous solution. J Pharm Sci 94(9):1928–1940. https://doi.org/10.1002/jps.20347
Boyd BM, Mudumba S, Farr SJ, inventors; Zogenix Inc., assignee (2005) Viscous formulations and their use in needle-free injection patent United States patent US8066661B2
Hooven MD (2018) Advanced delivery devices – sophisticated connected wearables: boosting biologics’ compliance, value & patient satisfaction. Drug Dev Deliv 16:24–31
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Vhora, I., Bardoliwala, D., Ranamalla, S.R., Javia, A. (2019). Parenteral Controlled and Prolonged Drug Delivery Systems: Therapeutic Needs and Formulation Strategies. In: Misra, A., Shahiwala, A. (eds) Novel Drug Delivery Technologies. Springer, Singapore. https://doi.org/10.1007/978-981-13-3642-3_7
Download citation
DOI: https://doi.org/10.1007/978-981-13-3642-3_7
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-3641-6
Online ISBN: 978-981-13-3642-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)