Abstract
Currently, full-thickness transplantation with human donor corneas is the most widely accepted treatment for corneal blindness. However, due to a severe shortage of human donor corneas as well as problems associated with the storage, screening, and immune response to allogeneic tissues, there has been a push to develop alternative therapies and materials for corneal tissue repair. Here, we review a range of stem cell-based therapies, prosthetics, and extracellular matrix-derived scaffolds, which have been utilized or are being developed for corneal regeneration in vitro, animal models, and human clinical trials.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Meek, K. M., & Knupp, C. (2015). Corneal structure and transparency. Progress in Retinal and Eye Research, 49, 1–16.
Jonas, J. B., & Holbach, L. (2005). Central corneal thickness and thickness of the lamina cribrosa in human eyes. Investigative Ophthalmology & Visual Science, 46, 1275–1279.
Maurice, D. M. (1957). The structure and transparency of the cornea. The Journal of Physiology, 136, 263–286.
McDermott, A. M. (2009). The role of antimicrobial peptides at the ocular surface. Ophthalmic Research, 41, 60–75.
Van Buskirk, E. M. (1989). The anatomy of the limbus. Eye, 3, 101–108.
Chen, S., Mienaltowski, M. J., & Birk, D. E. (2015). Regulation of corneal stroma extracellular matrix assembly. Experimental Eye Research, 133, 69–80.
Tuft, S. J., & Coster, D. J. (1990). The corneal endothelium. Eye, 4, 389–424.
Oliva, M. S., Schottman, T., & Gulati, M. (2012). Turning the tide of corneal blindness. Indian Journal of Ophthalmology, 60, 423–427.
Gain, P., Jullienne, R., He, Z., et al. (2016). Global survey of corneal transplantation and eye banking. JAMA Ophthalmology, 134, 167–173.
Williams, K. A., Esterman, A. J., Bartlett, C., Holland, H., Hornsby, N. B., Coster, D. J., et al. (2006). How effective is penetrating corneal transplantation? Factors influencing long-term outcome in multivariate analysis. Transplantation, 81, 896–901.
Lass, J. H., Benetz, B. A., Gal, R. L., Kollman, C., Raghinaru, D., Dontchev, M., et al. (2013). Donor age and factors related to endothelial cell loss ten years after penetrating keratoplasty: Specular Microscopy Ancillary Study. Ophthalmology, 120, 2428–2435.
Arenas, E., Esquenazi, S., Anwar, M., & Terry, M. (2012). Lamellar corneal transplantation. Survey of Ophthalmology, 57, 510–529.
Ikada, Y. (2006). Challenges in tissue engineering. Journal of the Royal Society Interface, 3, 589–601.
Chen, Y., Liao, C., Gao, M., Belin, M. W., Wang, M., Yu, H., et al. (2015). Efficacy and safety of corneal transplantation using corneas from foreign donors versus domestic donors: A prospective, randomized, controlled trial. Journal of Ophthalmology, 2015, 178289.
Dua, H. S., & Azuara-Blanco, A. (2000). Limbal stem cells of the corneal epithelium. Survey of Ophthalmology, 44, 415–425.
Dua, H. S., Gomes, J. A., & Singh, A. (1994). Corneal epithelial wound healing. The British Journal of Ophthalmology, 78, 401–408.
Tseng, S. G., Prabhasawat, P., Barton, K., Gray, T., & Meller, D. (1998). Amniotic membrane transplantation with or without limbal allografts for corneal surface reconstruction in patients with limbal stem cell deficiency. Archives of Ophthalmology, 116, 431–441.
Atallah, M. R., Palioura, S., Perez, V. L., & Amescua, G. (2016). Limbal stem cell transplantation: Current perspectives. Clinical Ophthalmology, 10, 593–602.
Baradaran-Rafii, A., Eslani, M., Haq, Z., Shirzadeh, E., Huvard, M. J., & Djalilian, A. R. (2017). Current and upcoming therapies for ocular surface chemical injuries. The Ocular Surface, 15, 48–64.
Holland, E. J. (2015). Management of limbal stem cell deficiency: A historical perspective, past, present, and future. Cornea, 34, S9–S15.
Ramachandran, C., Basu, S., Sangwan, V. S., & Balasubramanian, D. (2014). Concise review: The coming of age of stem cell treatment for corneal surface damage. Stem Cells Translational Medicine, 3, 1160–1168.
Vazirani, J., Mariappan, I., Ramamurthy, S., Fatima, S., Basu, S., & Sangwan, V. S. (2016). Surgical management of bilateral limbal stem cell deficiency. The Ocular Surface, 14, 350–364.
Thoft, R. A. (1977). Conjunctival transplantation. Archives of Ophthalmology, 95, 1425–1427.
Kenyon, K. R., & Tseng, S. C. (1989). Limbal autograft transplantation for ocular surface disorders. Ophthalmology, 96, 709–722 discussion 722–723.
Clearfield, E., Muthappan, V., Wang, X., & Kuo, I. C. (2016). Conjunctival autograft for pterygium. Cochrane Database of Systematic Reviews, 2, CD011349.
Rao, S. K., Rajagopal, R., Sitalakshmi, G., & Padmanabhan, P. (1999). Limbal autografting: Comparison of results in the acute and chronic phases of ocular surface burns. Cornea, 18, 164–171.
Holland, E. J., & Schwartz, G. S. (1996). The evolution of epithelial transplantation for severe ocular surface disease and a proposed classification system. Cornea, 15, 549–556.
Croasdale, C. R., Schwartz, G. S., Malling, J. V., & Holland, E. J. (1999). Keratolimbal allograft: Recommendations for tissue procurement and preparation by eye banks, and standard surgical technique. Cornea, 18, 52–58.
Kwitko, S., Marinho, D., Barcaro, S., Bocaccio, F., Rymer, S., Fernandes, S., et al. (1995). Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology, 102, 1020–1025.
Biber, J. M., Skeens, H. M., Neff, K. D., & Holland, E. J. (2011). The cincinnati procedure: Technique and outcomes of combined living-related conjunctival limbal allografts and keratolimbal allografts in severe ocular surface failure. Cornea, 30, 765–771.
Chan, C. C., Biber, J. M., & Holland, E. J. (2012). The modified Cincinnati procedure: Combined conjunctival limbal autografts and keratolimbal allografts for severe unilateral ocular surface failure. Cornea, 31, 1264–1272.
Espana, E. M., Di Pascuale, M., Grueterich, M., Solomon, A., & Tseng, S. C. G. (2004). Keratolimbal allograft in corneal reconstruction. Eye, 18, 406–417.
Basu, S., Sureka, S. P., Shanbhag, S. S., Kethiri, A. R., Singh, V., & Sangwan, V. S. (2016). Simple limbal epithelial transplantation: Long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology, 123, 1000–1010.
Sangwan, V. S., Basu, S., Macneil, S., & Balasubramanian, D. (2012). Simple limbal epithelial transplantation (SLET): A novel surgical technique for the treatment of unilateral limbal stem cell deficiency. The British Journal of Ophthalmology, 96, 931–934.
Vazirani, J., Ali, M. H., Sharma, N., Gupta, N., Mittal, V., Atallah, M., et al. (2016). Autologous simple limbal epithelial transplantation for unilateral limbal stem cell deficiency: Multicentre results. The British Journal of Ophthalmology, 100, 1416–1420.
Amescua, G., Atallah, M., Nikpoor, N., Galor, A., & Perez, V. L. (2014). Modified simple limbal epithelial transplantation using cryopreserved amniotic membrane for unilateral limbal stem cell deficiency. American Journal of Ophthalmology, 158, 469–475.
Rheinwald, J. G., & Green, H. (1975). Serial cultivation of strains of human epidermal keratinocytes: The formation of keratinizing colonies from single cells. Cell, 6, 331–343.
Pellegrini, G., Traverso, C. E., Franzi, A. T., Zingirian, M., Cancedda, R., & De Luca, M. (1997). Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. The Lancet, 349, 990–993.
Sangwan, V. S., Basu, S., Vemuganti, G. K., Sejpal, K., Subramaniam, S. V., Bandyopadhyay, S., et al. (2011). Clinical outcomes of xeno-free autologous cultivated limbal epithelial transplantation: A 10-year study. The British Journal of Ophthalmology, 95, 1525–1530.
Deshpande, P., Ramachandran, C., Sangwan, V. S., & Macneil, S. (2013). Cultivation of limbal epithelial cells on electrospun poly (lactide-co-glycolide) scaffolds for delivery to the cornea. In B. Wright & C. J. Connon (Eds.), Corneal regenerative medicine: Methods and protocols. Totowa, NJ: Humana Press.
Fasolo, A., Pedrotti, E., Passilongo, M., Marchini, G., Monterosso, C., Zampini, R., et al. (2016). Safety outcomes and long-term effectiveness of ex vivo autologous cultured limbal epithelial transplantation for limbal stem cell deficiency. The British Journal of Ophthalmology, 101(5), 640–649.
Rama, P., Bonini, S., Lambiase, A., Golisano, O., Paterna, P., De Luca, M., et al. (2001). Autologous fibrin-cultured limbal stem cells permanently restore the corneal surface of patients with total limbal stem cell deficiency. Transplantation, 72, 1478–1485.
Sangwan, V. S., Matalia, H. P., Vemuganti, G. K., Fatima, A., Ifthekar, G., Singh, S., et al. (2006). Clinical outcome of autologous cultivated limbal epithelium transplantation. Indian Journal of Ophthalmology, 54, 29–34.
Tsai, R. J.-F., Li, L.-M., & Chen, J.-K. (2000). Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. The New England Journal of Medicine, 343, 86–93.
Eslani, M., Baradaran-Rafii, A., & Ahmad, S. (2012). Cultivated limbal and oral mucosal epithelial transplantation. Seminars in Ophthalmology, 27, 80–93.
Nishida, K., Yamato, M., Hayashida, Y., Watanabe, K., Yamamoto, K., Adachi, E., et al. (2004). Corneal reconstruction with tissue-engineered cell sheets composed of autologous oral mucosal epithelium. The New England Journal of Medicine, 351, 1187–1196.
Nakamura, T., Inatomi, T., Sotozono, C., Amemiya, T., Kanamura, N., & Kinoshita, S. (2004). Transplantation of cultivated autologous oral mucosal epithelial cells in patients with severe ocular surface disorders. The British Journal of Ophthalmology, 88, 1280–1284.
Inatomi, T., Nakamura, T., Koizumi, N., Sotozono, C., Yokoi, N., & Kinoshita, S. (2006). Midterm results on ocular surface reconstruction using cultivated autologous oral mucosal epithelial transplantation. American Journal of Ophthalmology, 141, 267–275.
Prabhasawat, P., Ekpo, P., Uiprasertkul, M., Chotikavanich, S., Tesavibul, N., Pornpanich, K., et al. (2016). Long-term result of autologous cultivated oral mucosal epithelial transplantation for severe ocular surface disease. Cell and Tissue Banking, 17, 491–503.
Satake, Y., Higa, K., Tsubota, K., & Shimazaki, J. (2011). Long-term outcome of cultivated oral mucosal epithelial sheet transplantation in treatment of total limbal stem cell deficiency. Ophthalmology, 118, 1524–1530.
Dobrowolski, D., Wylegala, E., Wowra, B., & Orzechowska-Wylegala, B. (2011). Cultivated oral mucosa epithelium transplantation (COMET) in bilateral limbal stem cell deficiency. Acta Ophthalmologica. Supplement, 89. https://doi.org/10.1111/j.1755-3768.2011.4374.x
Sotozono, C., Inatomi, T., Nakamura, T., Koizumi, N., Yokoi, N., Ueta, M., et al. (2013). Visual improvement after cultivated oral mucosal epithelial transplantation. Ophthalmology, 120, 193–200.
Liu, J., Sheha, H., Fu, Y., Giegengack, M., & Tseng, S. C. (2011). Oral mucosal graft with amniotic membrane transplantation for total limbal stem cell deficiency. American Journal of Ophthalmology, 152, 739–47.e1.
Katikireddy, K. R., Dana, R., & Jurkunas, U. V. (2014). Differentiation potential of limbal fibroblasts and bone marrow mesenchymal stem cells to corneal epithelial cells. Stem Cells, 32, 717–729.
Zhang, L., Coulson-Thomas, V. J., Ferreira, T. G., & Kao, W. W. Y. (2015). Mesenchymal stem cells for treating ocular surface diseases. BMC Ophthalmology, 15, 155.
Meyer-Blazejewska, E. A., Call, M. K., Yamanaka, O., Liu, H., Schlötzer-Schrehardt, U., Kruse, F. E., et al. (2011). From hair to cornea: Towards the therapeutic use of hair follicle-derived stem cells in the treatment of limbal stem cell deficiency. Stem Cells, 29, 57–66.
Monteiro, B. G., Serafim, R. C., Melo, G. B., Silva, M. C. P., Lizier, N. F., Maranduba, C. M. C., et al. (2009). Human immature dental pulp stem cells share key characteristic features with limbal stem cells. Cell Proliferation, 42, 587–594.
Erbani, J., Aberdam, D., Larghero, J., & Vanneaux, V. (2016). Pluripotent stem cells and other innovative strategies for the treatment of ocular surface diseases. Stem Cell Reviews, 12, 171–178.
Hayashi, R., Ishikawa, Y., Ito, M., Kageyama, T., Takashiba, K., Fujioka, T., et al. (2012). Generation of corneal epithelial cells from induced pluripotent stem cells derived from human dermal fibroblast and corneal limbal epithelium. PLoS One, 7, e45435.
Kelaini, S., Cochrane, A., & Margariti, A. (2014). Direct reprogramming of adult cells: Avoiding the pluripotent state. Stem Cells Cloning, 7, 19–29.
Casaroli-Marano, R. P., Nieto-Nicolau, N., Martínez-Conesa, E. M., Edel, M., & Alvarez-Palomo, A. B. (2015). Potential role of induced pluripotent stem cells (IPSCs) for cell-based therapy of the ocular surface. Journal of Clinical Medicine, 4, 318–342.
Delmonte, D. W., & Kim, T. (2011). Anatomy and physiology of the cornea. Journal of Cataract and Refractive Surgery, 37, 588–598.
Beales, M. P., Funderburgh, J. L., Jester, J. V., & Hassell, J. R. (1999). Proteoglycan synthesis by bovine keratocytes and corneal fibroblasts: Maintenance of the keratocyte phenotype in culture. Investigative Ophthalmology & Visual Science, 40, 1658–1663.
Funderburgh, J. L., Mann, M. M., & Funderburgh, M. L. (2003). Keratocyte phenotype mediates proteoglycan structure: A role for fibroblasts in corneal fibrosis. The Journal of Biological Chemistry, 278, 45629–45637.
Karamichos, D., Funderburgh, M. L., Hutcheon, A. E. K., Zieske, J. D., Du, Y., Wu, J., et al. (2014). A role for topographic cues in the organization of collagenous matrix by corneal fibroblasts and stem cells. PLoS One, 9, e86260.
Du, Y., Funderburgh, M. L., Mann, M. M., Sundarraj, N., & Funderburgh, J. L. (2005). Multipotent stem cells in human corneal stroma. Stem Cells, 23, 1266–1275.
Du, Y., Sundarraj, N., Funderburgh, M. L., Harvey, S. A., Birk, D. E., & Funderburgh, J. L. (2007). Secretion and organization of a cornea-like tissue in vitro by stem cells from human corneal stroma. Investigative Ophthalmology & Visual Science, 48, 5038–5045.
Basu, S., Hertsenberg, A. J., Funderburgh, M. L., Burrow, M. K., Mann, M. M., Du, Y., et al. (2014). Human limbal biopsy-derived stromal stem cells prevent corneal scarring. Science Translational Medicine, 6, 266RA172–266RA172.
Joyce, N. C. (2003). Proliferative capacity of the corneal endothelium. Progress in Retinal and Eye Research, 22, 359–389.
Dapena, I., Ham, L., & Melles, G. R. J. (2009). Endothelial keratoplasty: DSEK/DSAEK or DMEK – The thinner the better? Current Opinion in Ophthalmology, 20, 299–307.
Proulx, S., Bensaoula, T., Nada, O., Audet, C., D’Arc Uwamaliya, J., Devaux, A., et al. (2009). Transplantation of a tissue-engineered corneal endothelium reconstructed on a devitalized carrier in the feline model. Investigative Ophthalmology & Visual Science, 50, 2686–2694.
De Araujo, A. L., & Gomes, J. Á. P. (2015). Corneal stem cells and tissue engineering: Current advances and future perspectives. World Journal of Stem Cells, 7, 806–814.
Proulx, S., & Brunette, I. (2012). Methods being developed for preparation, delivery and transplantation of a tissue-engineered corneal endothelium. Experimental Eye Research, 95, 68–75.
Kinoshita, S., Koizumi, N., Ueno, M., Okumura, N., Imai, K., Tanaka, H., Yamamoto, Y., Nakamura, T., Inatomi, T., Bush, J., Toda, M., Hagiya, M., Yokota, I., Teramukai, S., Sotozono, C., & Hamuro, J. (2018). Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. New England Journal of Medicine, 378, 995-1003.
Bostan, C., Theriault, M., Forget, K. J., Doyon, C., Cameron, J. D., Proulx, S., et al. (2016). In vivo functionality of a corneal endothelium transplanted by cell-injection therapy in a Feline model. Investigative Ophthalmology & Visual Science, 57, 1620–1634.
Koizumi, N., Okumura, N., Ueno, M., & Kinoshita, S. (2014). New therapeutic modality for corneal endothelial disease using rho-associated kinase inhibitor eye drops. Cornea, 33(Suppl 11), S25–S31.
Okumura, N., Okazaki, Y., Inoue, R., Kakutani, K., Nakano, S., Kinoshita, S., et al. (2016). Effect of the rho-associated kinase inhibitor eye drop (Ripasudil) on corneal endothelial wound healing. Investigative Ophthalmology & Visual Science, 57, 1284–1292.
Mccabe, K. L., Kunzevitzky, N. J., Chiswell, B. P., Xia, X., Goldberg, J. L., & Lanza, R. (2015). Efficient generation of human embryonic stem cell-derived corneal endothelial cells by directed differentiation. PLoS One, 10, e0145266.
Song, Q., Yuan, S., An, Q., Chen, Y., Mao, F. F., Liu, Y., et al. (2016). Directed differentiation of human embryonic stem cells to corneal endothelial cell-like cells: A transcriptomic analysis. Experimental Eye Research, 151, 107–114.
Zhang, K., Pang, K., & Wu, X. (2014). Isolation and transplantation of corneal endothelial cell-like cells derived from in-vitro-differentiated human embryonic stem cells. Stem Cells and Development, 23, 1340–1354.
Gomaa, A., Comyn, O., & Liu, C. (2010). Keratoprostheses in clinical practice – A review. Clinical & Experimental Ophthalmology, 38, 211–224.
Dohlman, C. H., Cruzat, A., & White, M. (2014). The Boston keratoprosthesis 2014: A step in the evolution of artificial corneas. Spektrum Augenheilkd, 28, 226–233.
Liu, C., Paul, B., Tandon, R., Lee, E., Fong, K., Mavrikakis, I., et al. (2005). The osteo-odonto-keratoprosthesis (OOKP). Seminars in Ophthalmology, 20, 113–128.
Iakymenko, S. (2013). Forty-five years of keratoprosthesis study and application at the Filatov Institute: A retrospective analysis of 1 060 cases. International Journal of Ophthalmology, 6, 375–380.
Colby, K. A., & Koo, E. B. (2011). Expanding indications for the Boston keratoprosthesis. Current Opinion in Ophthalmology, 22, 267–273.
Hicks, C. R., Crawford, G. J., Dart, J. K. G., Grabner, G., Holland, E. J., Stulting, R. D., et al. (2006). AlphaCor: Clinical outcomes. Cornea, 25, 1034–1042.
Hassanaly, S. I., Talajic, J. C., & Harissi-Dagher, M. (2014). Outcomes following Boston type 1 keratoprosthesis implantation in aniridia patients at the University of Montreal. American Journal of Ophthalmology, 158, 270–276.e1.
Ma, J. J., Graney, J. M., & Dohlman, C. H. (2005). Repeat penetrating keratoplasty versus the Boston keratoprosthesis in graft failure. International Ophthalmology Clinics, 45, 49–59.
Lee, W. B., Shtein, R. M., Kaufman, S. C., Deng, S. X., & Rosenblatt, M. I. (2015). Boston keratoprosthesis: Outcomes and complications. Ophthalmology, 122, 1504–1511.
Rudnisky, C. J., Belin, M. W., Guo, R., Ciolino, J. B., Dohlman, C. H., Aquavella, J., et al. (2016). Visual acuity outcomes of the Boston keratoprosthesis type 1: Multicenter study results. American Journal of Ophthalmology, 162, 89–98.
Aucoin, L., Griffith, C. M., Pleizier, G., Deslandes, Y., & Sheardown, H. (2002). Interactions of corneal epithelial cells and surfaces modified with cell adhesion peptide combinations. Journal of Biomaterials Science, Polymer Edition, 13, 447–462.
Bruining, M. J., Paul Pijpers, A., Kingshott, P., & Koole, L. H. (2002). Studies on new polymeric biomaterials with tunable hydrophilicity, and their possible utility in corneal repair surgery. Biomaterials, 23, 1213–1219.
George, A., & Pitt, W. G. (2002). Comparison of corneal epithelial cellular growth on synthetic cornea materials. Biomaterials, 23, 1369–1373.
Legeais, J.-M., & Renard, G. (1998). A second generation of artificial cornea (Biokpro II). Biomaterials, 19, 1517–1522.
Merrett, K., Griffith, C. M., Deslandes, Y., Pleizier, G., & Sheardown, H. (2001). Adhesion of corneal epithelial cells to cell adhesion peptide modified pHEMA surfaces. Journal of Biomaterials Science, Polymer Edition, 12, 647–671.
Noh, H. (2013). Enhanced cornea cell growth on a keratoprosthesis material immobilized with fibronectin or EGF. Macromolecular Research, 21, 169–175.
Jacob, J. T., Rochefort, J. R., Bi, J., & Gebhardt, B. M. (2005). Corneal epithelial cell growth over tethered-protein/peptide surface-modified hydrogels. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 72B, 198–205.
Wallace, C., Jacob, J. T., Stoltz, A., Bi, J., & Bundy, K. (2005). Corneal epithelial adhesion strength to tethered-protein/peptide modified hydrogel surfaces. Journal of Biomedical Materials Research. Part A, 72A, 19–24.
Johnson, G., Jenkins, M., Mclean, K. M., Griesser, H. J., Kwak, J., Goodman, M., et al. (2000). Peptoid-containing collagen mimetics with cell binding activity. Journal of Biomedical Materials Research, 51, 612–624.
Myung, D., Koh, W., Bakri, A., Zhang, F., Marshall, A., Ko, J., et al. (2007). Design and fabrication of an artificial cornea based on a photolithographically patterned hydrogel construct. Biomedical Microdevices, 9, 911–922.
Myung, D., Farooqui, N., Zheng, L. L., Koh, W., Noolandi, J., Cochran, J. R., et al. (2009). Bioactive interpenetrating polymer network hydrogels that support corneal epithelial wound healing. Journal of Biomedical Materials Research. Part A, 90, 70–81.
Myung, D., Duhamel, P.-E., Cochran, J., Noolandi, J., Ta, C., & Frank, C. (2008). Development of hydrogel-based keratoprostheses: A materials perspective. Biotechnology Progress, 24, 735–741.
Wilson, S. L., Sidney, L. E., Dunphy, S. E., Rose, J. B., & Hopkinson, A. (2013). Keeping an eye on decellularized corneas: A review of methods, characterization and applications. Journal of Functional Biomaterials, 4, 114–161.
Daoud, Y. J., Smith, R., Smith, T., Akpek, E. K., Ward, D. E., & Stark, W. J. (2011). The intraoperative impression and postoperative outcomes of gamma-irradiated corneas in corneal and glaucoma patch surgery. Cornea, 30, 1387–1391.
Zhang, M. C., Liu, X., Jin, Y., Jiang, D. L., Wei, X. S., & Xie, H. T. (2015). Lamellar keratoplasty treatment of fungal corneal ulcers with acellular porcine corneal stroma. American Journal of Transplantation, 15, 1068–1075.
Chen, S.-C., Telinius, N., Lin, H.-T., Huang, M.-C., Lin, C.-C., Chou, C.-H., et al. (2015). Use of Fish Scale-Derived BioCornea to seal full-thickness corneal perforations in Pig Models. PLoS One, 10, e0143511.
Nagai, T., Izumi, M., & Ishii, M. (2004). Fish scale collagen. Preparation and partial characterization. International Journal of Food Science & Technology, 39, 239–244.
Van Essen, T. H., Lin, C. C., Hussain, A. K., Maas, S., Lai, H. J., Linnartz, H., et al. (2013). A Fish Scale–Derived Collagen Matrix as artificial cornea in rats: Properties and potential fish-derived collagen matrix as artificial cornea. Investigative Ophthalmology & Visual Science, 54, 3224–3233.
Senthil, S., Rao, H. L., Babu, J. G., Mandal, A. K., & Garudadri, C. S. (2013). Comparison of outcomes of trabeculectomy with mitomycin C vs. ologen implant in primary glaucoma. Indian Journal of Ophthalmology, 61, 338–342.
Guo, X., Hutcheon, A. E. K., Melotti, S. A., Zieske, J. D., Trinkaus-Randall, V., & Ruberti, J. W. (2007). Morphological characterization of organized extracellular matrix deposition by ascorbic acid-stimulated human corneal fibroblasts. Investigative Ophthalmology & Visual Science, 48, 4050–4060.
Proulx, S., Uwamaliya, J. D. A., Carrier, P., Deschambeault, A., Audet, C., Giasson, C. J., et al. (2010). Reconstruction of a human cornea by the self-assembly approach of tissue engineering using the three native cell types. Molecular Vision, 16, 2192–2201.
Karamichos, D., Rich, C. B., Hutcheon, A. E. K., Ren, R., Saitta, B., Trinkaus-Randall, V., et al. (2011). Self-assembled matrix by umbilical cord stem cells. Journal of Functional Biomaterials, 2, 213–229.
Zhou, H.-X., Rivas, G., & Minton, A. P. (2008). Macromolecular crowding and confinement: Biochemical, biophysical, and potential physiological consequences. Annual Review of Biophysics, 37, 375–397.
Kumar, P., Satyam, A., Fan, X., Rochev, Y., Rodriguez, B. J., Gorelov, A., et al. (2014). Accelerated development of supramolecular corneal stromal-like assemblies from corneal fibroblasts in the presence of macromolecular crowders. Tissue Engineering Part C: Methods, 21, 660–670.
Boulze Pankert, M., Goyer, B., Zaguia, F., Bareille, M., Perron, M.-C., Liu, X., et al. (2014). Biocompatibility and functionality of a tissue-engineered living corneal stroma transplanted in the feline eye living corneal stroma transplanted in feline eye. Investigative Ophthalmology & Visual Science, 55, 6908–6920.
Wray, L. S., & Orwin, E. J. (2009). Recreating the microenvironment of the native cornea for tissue engineering applications. Tissue Engineering Part A, 15, 1463–1472.
Hayes, S., Lewis, P., Islam, M. M., Doutch, J., Sorensen, T., White, T., et al. (2015). The structural and optical properties of type III human collagen biosynthetic corneal substitutes. Acta Biomaterialia, 25, 121–130.
Rafat, M., Li, F., Fagerholm, P., Lagali, N. S., Watsky, M. A., Munger, R., et al. (2008). PEG-stabilized carbodiimide crosslinked collagen–chitosan hydrogels for corneal tissue engineering. Biomaterials, 29, 3960–3972.
Cheung, R. C. F., Ng, T. B., Wong, J. H., & Chan, W. Y. (2015). Chitosan: An update on potential biomedical and pharmaceutical applications. Marine Drugs, 13, 5156–5186.
Alaminos, M., Sánchez-Quevedo, M. A. D. C., Muñoz-Ávila, J. I., Serrano, D., Medialdea, S., Carreras, I., et al. (2006). Construction of a complete rabbit cornea substitute using a fibrin-agarose scaffold. Investigative Ophthalmology & Visual Science, 47, 3311–3317.
De La Cruz Cardona, J., Ionescu, A.-M., Gómez-Sotomayor, R., González-Andrades, M., Campos, A., Alaminos, M., et al. (2011). Transparency in a fibrin and fibrin–agarose corneal stroma substitute generated by tissue engineering. Cornea, 30, 1428–1435.
Garzón, I., Martín-Piedra, M. A., Alfonso-Rodríguez, C., González-Andrades, M., Carriel, V., Martínez-Gómez, C., et al. (2014). Generation of a biomimetic human artificial cornea model using Wharton’s jelly mesenchymal stem cells. Investigative Ophthalmology & Visual Science, 55, 4073–4083.
Fagerholm, P., Lagali, N. S., Merrett, K., Jackson, W. B., Munger, R., Liu, Y., et al. (2010). A biosynthetic alternative to human donor tissue for inducing corneal regeneration: 24-Month follow-up of a phase 1 clinical study. Sci. Transl. Med., 2, 46ra61.
Fagerholm, P., Lagali, N. S., Ong, J. A., Merrett, K., Jackson, W. B., Polarek, J. W., et al. (2014). Stable corneal regeneration four years after implantation of a cell-free recombinant human collagen scaffold. Biomaterials, 35, 2420–2427.
Hackett, J. M., Lagali, N., Merrett, K., Edelhauser, H., Sun, Y., Gan, L., et al. (2011). Biosynthetic corneal implants for replacement of pathologic corneal tissue: Performance in a Controlled Rabbit Alkali Burn Model. Investigative Ophthalmology & Visual Science, 52, 651–657.
Yumoto, H., Hirota, K., Hirao, K., Miyazaki, T., Yamamoto, N., Miyamoto, K., et al. (2015). Anti-inflammatory and protective effects of 2-methacryloyloxyethyl phosphorylcholine polymer on oral epithelial cells. Journal of Biomedical Materials Research. Part A, 103, 555–563.
Mclaughlin, C. R., Acosta, M. C., Luna, C., Liu, W., Belmonte, C., Griffith, M., et al. (2010). Regeneration of functional nerves within full thickness collagen–phosphorylcholine corneal substitute implants in guinea pigs. Biomaterials, 31, 2770–2778.
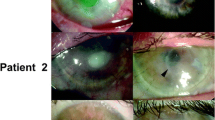
Buznyk, O., Pasyechnikova, N., Islam, M. M., Iakymenko, S., Fagerholm, P., & Griffith, M. (2015). Bioengineered corneas grafted as alternatives to human donor corneas in three high-risk patients. Clinical and Translational Science, 8, 558–562.
Mirazul Islam, M., Cepla, V., He, C., Edin, J., Rakickas, T., Kobuch, K., et al. (2015). Functional fabrication of recombinant human collagen-phosphorylcholine hydrogels for regenerative medicine applications. Acta Biomaterialia, 12, 70–80.
Villa-Diaz, L. G., Ross, A. M., Lahann, J., & Krebsbach, P. H. (2013). The evolution of human pluripotent stem cell culture: From feeder cells to synthetic coatings. Stem Cells, 31, 1–7.
Gouveia, R. M., Jones, R. R., Hamley, I. W., & Connon, C. J. (2014). The bioactivity of composite Fmoc-RGDS-collagen gels. Biomaterials Science, 2, 1222–1229.
Miotto, M., Gouveia, R. M., & Connon, C. J. (2015). Peptide amphiphiles in corneal tissue engineering. Journal of Functional Biomaterials, 6, 687–707.
Gouveia, R. M., Hamley, I. W., & Connon, C. J. (2015). Bio-fabrication and physiological self-release of tissue equivalents using smart peptide amphiphile templates. Journal of Materials Science. Materials in Medicine, 26, 242.
Uzunalli, G., Soran, Z., Erkal, T. S., Dagdas, Y. S., Dinc, E., Hondur, A. M., et al. (2014). Bioactive self-assembled peptide nanofibers for corneal stroma regeneration. Acta Biomaterialia, 10, 1156–1166.
O’Leary, L. E. R., Fallas, J. A., Bakota, E. L., Kang, M. K., & Hartgerink, J. D. (2011). Multi-hierarchical self-assembly of a collagen mimetic peptide from triple helix to nanofibre and hydrogel. Nature Chemistry, 3, 821–828.
Islam, M. M., Ravichandran, R., Olsen, D., Ljunggren, M. K., Fagerholm, P., Lee, C. J., et al. (2016). Self-assembled collagen-like-peptide implants as alternatives to human donor corneal transplantation. RSC Advances, 6, 55745–55749.
Bareiss, B., Ghorbani, M., Li, F., Blake, J. A., Scaiano, J. C., Zhang, J., et al. (2010). Controlled release of acyclovir through bioengineered corneal implants with silica nanoparticle carriers. The Open Tissue Engineering and Regenerative Medicine Journal, 3, 10–17.
Riau, A. K., Mondal, D., Aung, T. T., Murugan, E., Chen, L., Lwin, N. C., et al. (2015). Collagen-based artificial corneal scaffold with anti-infective capability for prevention of perioperative bacterial infections. ACS Biomaterials Science & Engineering, 1, 1324–1334.
Alarcon, E. I., Vulesevic, B., Argawal, A., Ross, A., Bejjani, P., Podrebarac, J., et al. (2016). Coloured cornea replacements with anti-infective properties: Expanding the safe use of silver nanoparticles in regenerative medicine. Nanoscale, 8, 6484–6489.
Islam, M. M., Buznyk, O., Reddy, J. C., Pasyechnikova, N., Alarcon, E. I., Hayes, S., Lewis, P., Fagerholm, P., He, C., Iakymenko, S., Liu, W., Meek, K. M., Sangwan, V. S., & Griffith, M. (2018) Biomaterials-enabled cornea regeneration in patients at high risk for rejection of donor tissue transplantation. npj Regenerative Medicine, 3, 2.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
McTiernan, C.D., Brunette, I., Griffith, M. (2018). Stem Cell Therapy and Regenerative Medicine in the Cornea. In: Ballios, B., Young, M. (eds) Regenerative Medicine and Stem Cell Therapy for the Eye. Fundamental Biomedical Technologies. Springer, Cham. https://doi.org/10.1007/978-3-319-98080-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-98080-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98079-9
Online ISBN: 978-3-319-98080-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)